US Pharm.
2008;33(9):Epub.
Alcoholism (or alcohol
dependence) is a chronic disease of the brain.1,2 Left
untreated, alcoholism is progressive and may be life threatening.1
This disease is characterized by relapse similar to other conditions such as
diabetes, hypertension, or asthma.2,3
According to the National
Epidemiologic Survey on Alcohol Related Disorders, in a study conducted by the
National Institute on Alcohol Abuse and Alcoholism, from 2001 through 2002,
5.42% of U.S. males and 2.32% of U.S. females suffered from this disorder.4
It is estimated that 10% to 20% of men and 5% to 10% of women will suffer from
alcoholism sometime in their lives, depending which criteria are used to
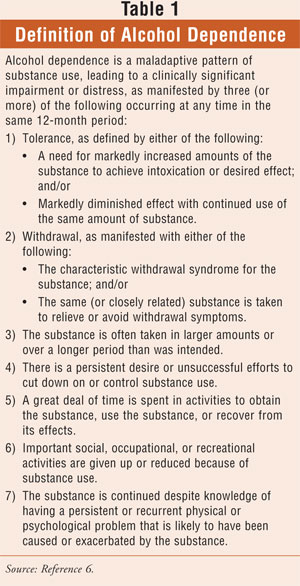
define alcoholism.5 The Diagnostic and Statistical Manual of
Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) defines
alcohol dependence based on the presence of several criteria, which are
described in TABLE 1.6
Some of the nonspecific
symptoms of alcoholism include insomnia, depression, anxiety, gastrointestinal
problems, sexual dysfunction, and severe premenstrual syndrome. Upon physical
examination, a physician might find hypertension, spider angiomata, acne
rosacea, liver disease, and/or portal hypertension. An alcoholic's medical
history may be positive for past trauma, eating disorders, depression, anxiety
disorders, sexual or physical abuse, and/or gynecologic disorders.7
Risk Factors
A family history of
alcoholism is a strong risk factor for the disease.8 Studies have
shown that first-degree relatives (i.e., parents, siblings, children) of
alcoholics are two to four times more likely to develop alcoholism than those
who do not have relatives with the disease.8 The reason for this is
twofold--a genetic component to alcoholism and the shared family environment.4,8
There is evidence that points to a heritability rate of 50% to 60%.4,8
Family dynamics and other shared features of a family's history (e.g.,
financial, social, educational) can contribute to developing an alcohol-use
disorder.
Stress is a common denominator
among female alcoholics.1,9,10 Drinking to cope with stressors is a
risk factor for developing alcoholism, and that should be examined in women
who may have a propensity to progress to alcoholic drinking. Having a history
of abuse of any sort--sexual, physical, or emotional--is another strong risk
factor for developing alcohol dependence.1,9
Troubled relationships
with close family members may lead to alcoholism, particularly in women.1,10
Peer pressure also contributes to the risk of developing alcohol dependence.9
Women whose significant others drink heavily are more likely to become
alcoholics than women who are not exposed to heavy drinking.1,10
Alcohol Dependence in Women
Female alcoholics
experience a different course of disease development and suffer differing
consequences than men.11,12 Fewer women drink than men,1,8,13
and women are more likely to be abstinent from alcohol throughout their
lifetime than men.14,15 However, this pattern is changing among
young women.13 Binge drinking among adolescent and college-age
females is on the rise, which is problematic because of the number of adverse
events that result from this.15
The way women drink and the
reasons women drink also differ from those of men.14,15 Women often
drink because of the stresses of the various roles they have in life, such as
wife, mother, and employee.15 They often drink alone, binge less,
have regular patterns of use (at different times of the day), and drink less
alcohol than men.15 They will often consume a different type of
alcoholic beverage than men as well.14
Alcoholism presents
differently in women than in men.13 Women often start drinking at
an older age, yet the progression from first drink to alcohol dependency
progresses much more quickly in women than in men.7,9,12,14,16 This
phenomenon is known as telescoping.15 Women tend to start
drinking at lower doses and consume less than men overall.13,15
Despite this, women develop medical and psychological consequences more
severely and more quickly after the beginning of heavy consumption of alcohol.1,13,15
In fact, evidence shows that women suffer a 50% to 100% higher death rate from
alcohol than men. Reasons for death include suicide, accidents, and medical
complications, such as liver and/or heart disease.1,15 Despite the
greater frequency and severity of medical issues, women experience fewer and
less severe withdrawal symptoms.
Women are more vulnerable to
the effects of alcohol than men.1,9,17 They are more likely to
develop organ damage, even though they may have been drinking less or for a
shorter time than men.1,9,16,18 More women who were diagnosed with
alcohol dependency also had dependency on another substance.15
Women suffer different
psychosocial problems due to alcohol dependence. They are more likely to
suffer damaged relationships and emotional problems than men. Emotional issues
cause so much morbidity in the female alcoholic that a negative mood is highly
associated with cravings and is an important risk factor for relapse.3
Much of this stems from the stigma attached to women and alcoholism.9
For this reason, alcoholic women are more likely to seek treatment in a
primary care or psychiatric setting for physical illness and marital or
emotional problems.14,19
Pharmacokinetics: Women
versus Men
The
pharmacokinetics are different in women than in men.20 When women
and men are administered the same quantity of ethanol per kilogram of body
weight, women show a higher blood alcohol concentration (BAC).7,13,15,21
This increase in bioavailability may contribute to the higher vulnerability of
women to the toxic effects of ethanol.17 There are several factors
that may contribute to the higher BAC in women.
When an equivalent dose of
alcohol is administered to both sexes IV, the BAC is identical. However, when
an equivalent dose is administered orally, the resulting BAC is higher in
women.18,21 This suggests that first-pass metabolism (FPM) is
smaller in females.
Unlike other drugs, FPM of
ethanol is not dependent solely on the liver, but rather on metabolism in the
gastric mucosa.18,21 Ethanol is metabolized by alcohol
dehydrogenase (ADH) into acetaldehyde, which is toxic.15,18,21 (A
hangover is due in part to a buildup of acetaldehyde.) Acetaldehyde is further
metabolized to acetate by ADH in the liver.18 Lower levels of ADH
in women, particularly in the stomach, result in a lower FPM.7,9,15,21,22
A decreased FPM is one factor contributing to an increased BAC in women
compared to men.
Another reason for the
observed higher ethanol concentration in women versus men may be the volume of
distribution (VD). Baraona et al found the VD to be 7.3% lower in women,
although they concluded that the lower VD is not large enough to account for
the higher BAC.21 Despite Baraona's conclusion, it appears that the
smaller VD in women may contribute to higher alcohol concentrations.9,12,15
Ethanol is a water-soluble molecule.18 Because women have more
fatty tissue and 12% less body water than men, the VD is smaller in women.9,12,15,18
Gastric emptying influences
the concentration of ethanol. Accelerated gastric emptying results in less
exposure to ADH in the gastric mucosa, thus decreasing the FPM effect. In both
sexes, fasting results in an increased rate of gastric emptying and
consequently a smaller FPM. Women have a 43% faster gastric emptying in
response to alcohol than men.18 This decreases exposure to ADH in
the stomach, thereby decreasing the FPM.
A final difference in the
pharmacokinetics of ethanol in women is the rate of metabolism and
elimination. Women eliminate alcohol from their body faster than men.15,20,21
This seems counterintuitive to resulting in an increased concentration of
alcohol, but it may partially explain the higher toxicity women experience
from the drug. Since the first metabolite of ethanol breakdown (acetaldehyde)
is toxic, a faster metabolism may result in greater medical sequelae. Longer
exposure to acetaldehyde may contribute to the greater toxicity in women.18,20
Although the actual mechanism responsible for the higher rate of elimination
in women remains unknown, it is postulated that gonadal hormones (i.e.,
progesterone, testosterone, estrogen) may play a role.20
Alcohol's Effects on
Physical and Mental Health
Women's increased
vulnerability to alcohol leads to quicker and, in many cases, more severe
consequences. Their risk of morbidity and mortality is increased.9,15,16
Alcoholics are at a higher risk of developing heart disease, brain disease,
liver disease, muscle wasting, bone disease, hypertension, stroke, and cancer,
as well as metabolic disorders.1,13,14,16,18
Both male and female
alcoholics are at an increased risk of cardiomyopathy.7,12,15 This
may be due to alcoholic-induced hypertension or free radicals.7 The
incidence of cardiomyopathy is the same in men and women. However, women
develop heart disease after a shorter exposure time to, and overall lower
consumption of, alcohol.12,15
Both men and women who abuse
alcohol experience a decrease in cognitive performance. With women, though, it
appears earlier and with less alcohol exposure than with men.9,11,12,15
CT scans have revealed a decreased brain volume in alcoholics.11 A
study conducted by Mann et al demonstrated a decrease in brain volume and an
increase in cerebrospinal fluid.12 Again, with female alcoholics,
this brain pathology develops after a shorter period of heavy drinking and an
overall lower alcohol exposure than with male alcoholics.11
Evidence shows that the "brain shrinkage" is reversible upon abstinence from
alcohol.11,12
Alcohol-induced liver damage
may occur in any alcoholic. Both men and women are susceptible to liver
injury. In women, alcoholic liver disease may be more severe with less alcohol
consumption.9,12,14 It is estimated that women who drink 20 to 40 g
of ethanol (approximately 2-4 drinks) per day are at the same risk as men who
drink 60 to 80 g per day.11
Chronic heavy drinking is
associated with an increased risk of bone fracture.7,17 This may be
due to a greater risk of falling and/or to ethanol's effects on bone.7
Evidence shows that both male and female alcoholics have a higher risk of
osteoporosis than nonalcoholics. The mechanisms involved appear to be due to
both direct effects on the bone and bone marrow cells and indirect effects via
endocrine disruption.17 Evidence shows that in females,
ethanol-induced bone loss results from both the inhibition of bone formation
(via inhibition of osteoblastogenesis) and the induction of bone resorption
(via stimulated osteoclastogenesis).17
Heavy alcohol consumption may
result in muscle wasting. The degree of muscle atrophy that results from
chronic ethanol consumption is directly related to the duration and amount of
alcohol ingested. Fortunately, like brain atrophy, alcohol-induced muscle
atrophy is reversible once abstinence from alcohol is achieved.1
Alcohol use promotes the
development of certain cancers.1 Cancers of the digestive system,
head and neck (especially in smokers), and breast have been associated with
ethanol consumption.1 Alcohol disrupts hormonal cycles in males and
in females.17 As a result, the female sex hormone balance becomes
altered and an increased risk in breast cancer results.7,9,15,23
One study showed that women who drank 2.5 to 5 drinks daily (on average) had a
40% higher incidence of breast cancer than nondrinkers. In fact, this risk
climbed by 9% for each 10-g increase (about 1 drink) in daily alcohol
consumption up to 60 g per day.7 The mechanism for increased risk
of breast cancer may be ethanol's effect on estradiol after acute ingestion.9,2
The hormonal imbalances
created by chronic alcohol abuse create reproductive dysfunction as well.9,15,17,23
In females, the gonadal hormone imbalance may lead to infertility,
miscarriage, and spontaneous abortion.9,15,23 The menstrual cycle
may become irregular, resulting in anovulation, amenorrhea, luteal phase
dysfunction, and hyperprolactemia.15,23
Women present with a higher
incidence of psychosocial problems than men, and female alcoholics' comorbid
psychiatric diagnoses differ from those of men.7,8,14,19 Female
alcoholics are at a higher risk for being victims of domestic violence and
rape, which may result in posttraumatic stress disorder.7,15,19
This may be why they are four times more likely to attempt suicide than
nonalcoholic women.7 Women who abuse alcohol experience more
relationship problems, including marital issues.7,14 Compared to
men, who suffer more from antisocial behavior and comorbid abuse of other
drugs,8,19 women are more likely to suffer from depression,
anxiety, mania, phobic disorders, and eating disorders.7,9,12,19
Fetal Alcohol Syndrome
Alcohol consumption
during pregnancy is the leading preventable cause of birth defects and
mental/developmental problems.1,7,15,24 Many women, from all walks
of life, drink during pregnancy. It is estimated that anywhere from 14% to
22.5% of women report some alcohol use while pregnant.25 These
figures are likely to be low, as the stigma of drinking during pregnancy may
prevent women from reporting it. Heavy binge or chronic prenatal exposure to
alcohol causes fetal alcohol syndrome (FAS).15,18 There is evidence
that suggests that in the early weeks of gestation, the fetus may be more
vulnerable to developing FAS.15 Since the "safe" amount of alcohol
and the "safe" stage of pregnancy to drink are unknown (if they exist at all),
pregnant women are urged not to drink at all during pregnancy.1
FAS is defined by four
criteria: 1) maternal drinking, 2) low birth weight, 3) characteristic facial
anomalies, and 4) abnormal neurologic development.15,24 The facial
features on FAS individuals may include any combination of the following: thin
upper lip, smooth philtrum, flat midface, small eyes, and epicanthal folds.15,24
The brain damage that results from FAS may lead to lifelong problems with
learning, memory, attention, and problem solving.1
There may be some mental,
behavioral, and physical problems due to prenatal alcohol exposure, even
without an FAS diagnosis. The terms alcohol-related neurodevelopmental
disorder (ARND) and fetal alcohol spectrum disorder (FASD) have
been used to describe the presence of abnormalities caused by drinking while
pregnant.15,24 Defects in the bone, heart, kidney, and vision or
hearing systems are symptoms of FASD.15 Low IQ scores and learning
disabilities result from maternal drinking prenatally. Behavioral problems
such as overactive disorders and attention-deficit disorders have been
associated with fetal alcohol exposure.24
Medications
Alcoholism is still
viewed by some as a character defect and not a treatable disease.3
In addition to psycho behavioral therapy, there are medications being used to
treat alcoholism. Medications are used for acute withdrawal as well as for
maintaining sobriety.22
Acute alcohol withdrawal (AW)
is characterized by many symptoms. They are not always all present, but they
may occur in any combination. They are "disturbance of consciousness, change
in cognition or perceptual disturbance developing in a short period,"
hyperpyrexia, hypertension, tachycardia, diaphoresis, nausea, headache, and
delirium tremens (DTs).22,26 These symptoms occur during withdrawal
or slightly after.26 However, DTs do not develop for two to three
days after acute withdrawal, and they usually last for 48 to 72 hours. DTs are
serious and may result in death; however, with the proper medical management,
mortality rates have fallen to 0% to 1%.2
The first-line treatment of AW
is sedative hypnotics, particularly benzodiazepines.22,26 Women
have a robust response to benzodiazepines and may require lower doses;
however, for AW the doses are larger than those prescribed for anxiety.22,26
Although not recommended as sole pharmacotherapy for AW, neuroleptics (i.e.,
haloperidol, chlorpromazine, and promazine) may be used in conjunction with
benzodiazepines.26 Adrenergic agonists, such as clonidine, may be
used in conjunction as well, especially for controlling hypertension and
tachycardia.26
There are three FDA-approved
medications for maintaining sobriety: disulfiram, naltrexone, and acamprosate (TABLE
2). Disulfiram is an aversive agent. It inhibits aldehyde dehydrogenase
and prevents acetaldehyde from being further metabolized.2,3,22
Disulfiram does not decrease cravings, so the motivation to continue
abstinence is due to the resultant adverse effects when alcohol is consumed.2,27
The buildup of acetaldehyde causes flushing, sweating, dyspnea, tachycardia,
headache, and nausea.2,3 Side effects are usually fatigue and
metallic taste, but they can be serious and include elevated hepatic enzymes
or hepatotoxicity, depression, and psychotic reactions.2,22,27
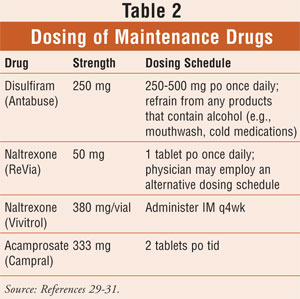
Naltrexone is an anticraving
medication that antagonizes the mu opioid receptors.2,3,22,28,29
Alcohol releases the endogenous opioid peptides, thereby stimulating opioid
receptors.3,22 Naltrexone decreases the incidence of relapse and
heavy drinking. However, it is associated with adverse effects that may affect
compliance rates.28,29 Side effects include nausea, abdominal
cramps, tearfulness, restlessness, bone or joint pain, myalgia, and nasal
symptoms. Because naltrexone has been known to cause hepatocellular injury, it
is contraindicated in patients with acute hepatitis or liver failure.28,29
A depot formulation of
naltrexone was developed and released in 2006 under the promise of reducing
adverse events, improving compliance, and improving therapeutic outcome
through constant therapeutic levels.2,3,27,28 Contrary to
expectations, the naltrexone depot formulation caused the same, and possibly
more severe, adverse events as the oral formulation.2,28 In
addition to the side effects caused by oral naltrexone, the depot injection
also causes tenderness, pain, induration, angioedema, inflammation, and
contusion in approximately 15% of patients.28
Acamprosate may benefit
alcoholic patients with anxiety, a negative family history of alcoholism, and
late age of onset.2 Acamprosate is used to alleviate craving and
restore brain function.3 Acamprosate was approved by the FDA based
largely on efficacy data from European studies.2 However, the
efficacy of acamprosate has come into question. There have been U.S. studies
that have not demonstrated the efficacy of the drug.2,30 The common
side effects of acamprosate are diarrhea, nervousness, and fatigue.2
Even though these three drugs
have been known to be effective in maintaining abstinence, behavioral
intervention along with drug therapy results in a more favorable outcome.
Psychotherapy combined with medical management increases abstinence by
approximately 20%.30
Role of the Pharmacist
Since alcoholism is
associated with high morbidity and mortality rates, it is imperative that
pharmacists take advantage of their role in the health care continuum to
improve patients' treatment outcomes. As noncompliance is a problem with
alcoholism treatments,27 the pharmacist can monitor refills and
counsel patients on the need to take their medications as prescribed. If the
patient is experiencing adverse effects that may affect compliance, the
pharmacist can help the patient and physician choose an alternative treatment
that is more tolerable. Of equal importance to compliance is the prevention of
FAS. The pharmacist must tactfully discuss FAS with women, stressing the
importance of avoiding alcohol while pregnant or avoiding pregnancy while
drinking.
REFERENCES
1. Alcohol: A
Women's Health Issue. Rockville, MD: National Institutes of Health,
National Institute on Alcohol Abuse and Alcoholism; 2003. NIH publication No.
03-4956. http://pubs.niaaa.nih.gov/publications/brochurewomen/women.htm.
Accessed July 1, 2008.
2. Johnson BA. Update
on neuropharmacological treatments for alcoholism: scientific basis and
clinical findings. Biochem Pharmacol. 2008;75:34-56.
3. Hellig M, Egli M.
Pharmacologic treatment of alcohol dependence: target symptoms and target
mechanisms. Pharmacol Ther. 2006;111:855-876.
4. National
Epidemiologic Survey on Alcohol and Related Conditions (NESARC). National
Institute on Alcohol Abuse and Alcoholism. www.nesarc.niaaa.nih.gov. Accessed
July 16, 2008.
5. Alcoholism.
Encyclopedia Britannica Online. 2008.
http://original.britannica.com/eb/article-251754/alcoholism. Accessed July 16,
2008.
6. American Psychiatric
Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed,
Text Revision (DSM-IV-TR). Washington, DC: American Psychiatric
Association; 2000.
7. Cyr MG, McGarry KA.
Alcohol use disorders in women. Screening methods and approaches to treatment. Postgrad
Med.2002;112:31-32,39-40,43-47.
8. Prescott CA. Sex
differences in the genetic risk for alcoholism. Alcohol Res Health. 2002;26:264-273.
9. Van der Walde H,
Urgenson FT, Weltz SH, Hanna FJ. Women and alcoholism: a biopsychosocial
perspective and treatment approaches. J Counsel Dev. 2002;80:145-153.
10. Timko C, Finney
JW, Moos RH. The 8-year course of alcohol abuse: gender differences in social
context and coping. Alcohol Clin Exp Res. 2005;29:612-621.
11. Mann K, Batra A,
Günthner, Schroth G. Do women develop alcohol brain damage more readily than
men? Alcohol Clin Exp Res. 1992;16:1052-1056.
12. Mann K, Ackermann
K, Croissant B, et al. Neuroimaging of differences in alcohol dependence: are
women more vulnerable than men? Alcohol Clin Exp Res. 2005;29:896-901.
13. Becker JB, Hu M.
Sex differences in drug abuse. Front Neuroendocrinol. 2008;29:36-47.
14. Green CA, Perrin
NA, Polen MR. Gender differences in relationships between multiple measures of
alcohol consumption and physical and mental health. Alcohol Clin Exp Res. 2004;28:754-764.
15. Greenfield SF,
Manwani SG, Nargiso JE. Epidemiology of substance use disorders in women. Obstet
Gynecol Clin North Am.2003;30:413-446.
16. Diehl A, Croissant
B, Batra A, et al. Alcoholism in women: is it different in onset and outcome
compared to men? Eur Arch Psychiatry Clin Neurosci. 2007;257:344-351.
17. Ronis MJ, Wands JR,
Badger TM, et al. Alcohol-induced disruption of endocrine signaling. Alcohol
Clin Exp Res. 2007;31:1269-1285.
18. Lieber C, Abittan
C. Pharmacology and metabolism of alcohol, including its metabolic effects and
interactions with other drugs. Clin Derm. 1999;17:365-379.
19.
Zilberman ML, Tavares H,
Blume SB, el-Guebaly N. Substance use disorders: sex differences and
psychiatric comorbidity. Can J Psychiatry. 2003;48:1-13.
20. Dettling A, Skopp
G, Graw M, Haffner HT. The influence of sex hormones on the elimination
kinetics of ethanol. Forensic Sci Int. 2008;177:85-89.
21. Baraona E, Abittan
CS, Dohmen K, et al. Gender differences in pharmacokinetics of alcohol. Alcohol
Clin Exp Res. 2001;25:502-507.
22. Bogenschutz MP,
Geppert CM. Pharmacologic treatments for women with addictions. Obstet
Gynecol Clin North Am. 2003;30:523-544.
23. Sarkola T, Mäkisalo
H, Fukunaga T, Erikson CJ. Acute effect of alcohol on estradiol, estrone,
progesterone, prolactin, cortisol, and luteinizing hormone in premenopausal
women. Alcohol Clin Exp Res. 1999;23:976-982.
24. Bailey BA, Sokol
RJ. Pregnancy and alcohol use: evidence and recommendations for prenatal care. Clin
Obstet Gynecol. 2008;51:436-444.
25. Screening for
alcohol use and alcohol-related problems. Alcohol Alert. 2005;65:1-8.
Rockville, MD: National Institutes of Health, National Institute on Alcohol
Abuse and Alcoholism. http://pubs.niaaa.nih.gov/publications/aa65/AA65.htm.
Accessed July 14, 2008.
26. Mayo-Smith MF,
Beecher LH, Fischer TL, et al. Management of alcohol withdrawal delirium. Arch
Intern Med. 2004;164:1405-1412.
27. Peterson AM.
Improving adherence in patients with alcohol dependence: a new role for
pharmacists. Am J Health Syst Pharm. 2007;64(suppl 3):S23-S29.
28. Roozen H, de Waart
R, van den Brink W. Efficacy and tolerability of naltrexone in the treatment
of alcohol dependence: oral versus injectable delivery. Eur Addict Res.
2007;13:201-206.
29. Naltrexone
hydrochloride tablets package insert. St. Louis, MO: Mallinckrodt; September
2003.
30. Anton RF, O'Malley
SS, Ciraulo DA, et al. Combined pharmacotherapies and behavioral interventions
for alcohol dependence: the COMBINE study. JAMA. 2006;295:2003-2017.
31. Rakel R, Bope E. Conn's
Current Therapy. 60th ed. St. Louis, MO: WB Saunders; 2008.
To comment on this article, contact
rdavidson@jobson.com.





