US Pharm. 2007;32(10):44-50.
Pneumonia is an infectious inflammation of
the lung by bacteria, viruses, and other organisms. Community-acquired
pneumonia (CAP) has been defined as an infection of the lungs in a patient who
is not hospitalized or who has resided in a long-term care facility for 14
days prior to the onset of symptoms; this infection is associated with at
least some signs and symptoms of acute infection and is accompanied by the
presence of an acute infiltrate on chest radiograph.1 Despite
advances in antibiotic therapy, medical techniques, and access to medical
care, CAP continues to be a leading cause of morbidity and mortality in the
adult population of the United States. Currently, pneumonia and influenza
together are ranked as the eighth leading cause of death in the U.S.2
In 2004, a total of 59,664 Americans died of pneumonia. The highest rate of
pneumonia is seen in people older than 65 years.3 Pneumonia and
influenza together represented a cost to the U.S. economy in 2004 of $37.5
billion; $5.6 billion was due to indirect mortality costs and $31.9 billion
was due to direct costs.4
Pneumonia guidelines have been
published by the American Thoracic Society (ATS) and the Infectious Diseases
Society of America (IDSA) as well as numerous other organizations. In order to
reduce confusion associated with multiple sources of information, the ATS and
IDSA convened a joint committee to develop a unified CAP guideline document;
the new guidelines were published in early 2007.5 This review
discusses how CAP occurs, which infectious bacteria cause pneumonia, how
pneumonia presents, how it is diagnosed and how to treat it according to the
current guidelines.
Pathophysiology
The lungs are
continuously exposed to the mixture of gases, particles, and microbes that are
in the air we breath.6 The lower airways, where a pneumonia will
occur, are likely to remain sterile due to the normal host-defenses of the
lungs. Infectious agents can gain access to the lower respiratory tract via
microaspirations of oropharyngeal contents (a common occurrence in both
healthy and sick people during sleep), inhalation of aerosolized material,
and, less commonly, directly from the blood. Pneumonias occur when the normal
host-defenses are overwhelmed, when a particularly virulent organism is
present, or when a large amount of organism is there.
Common Bacterial Causes of
CAP
Numerous organisms
can cause CAP. The particular causative agent may change according to the site
of acquisition of illness, patient comorbidities, and immune status. Table 1
lists the most common pathogens in CAP, in decreasing order of occurrence and
by severity of illness as judged by site of care (ambulatory vs. hospitalized).
5 Streptococcus pneumoniae is the most likely pathogen to cause a
pneumonia infection in an ambulatory patient in the community.5,7,8
Another gram-positive organism that can cause pneumonia is Staphylococcus
aureus, although this bacterium is more liable to be associated with
influenza outbreaks or with CAP patients requiring an ICU admission.5,7
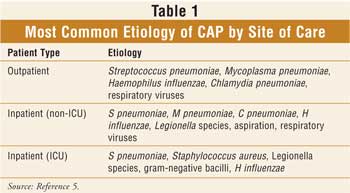
Gram-negative bacteria, such
as Haemophilus influenzae and Moraxella catarrhalis, can occur
and are most likely seen in those patients who have underlying
bronchopulmonary disease.5 Risks of infection from more serious
gram-negative species, such as Enterobacteriaceae species and
Pseudomonas aeruginosa, may occur with chronic oral steroid administration
or severe underlying bronchopulmonary disease, alcoholism, and frequent
antibiotic therapy.9,10 Finally, atypical organisms, such as
Mycoplasma pneumoniae and Chlamydia pneumoniae, are common causes
of pneumonia, especially among outpatients and young adults.5,11
Signs and Symptoms
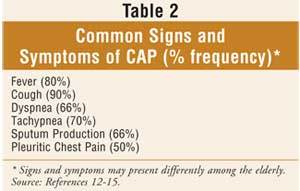
Patients with CAP
usually present with fever and a brief history of respiratory problems such as
cough, dyspnea, tachypnea, sputum production, and pleuritic chest pain.
12,13 Elderly patients may be less likely to present with standard
symptoms of CAP (e.g., cough, fever) and may actually present with confusion
and an altered mental status.14 Most patients with CAP will have a
focal lung examination, with findings ranging from crackles to bronchial
breath sounds (very loud, high-pitched sounds via stethoscope).15
Table 2 describes common signs and symptoms of CAP and the frequency with
which they may occur.
Diagnosis of CAP
In addition to
signs and symptoms, a definitive infiltrate on chest x-ray (or another imaging
technique) is required for the diagnosis of pneumonia.5 X-ray is
also necessary to allow differentiation between CAP and other causes of cough
and fever.5 Supporting microbiological evidence is usually not
required for the diagnosis. Extra diagnostic tests (e.g., sputum culture,
blood cultures, Legionella urine antigen test, pneumococcal urine antigen
test) may be completed when the result is likely to change empiric therapy,
when the test is likely to have a high yield, when the patient is
hospitalized, or if the patient is critically ill with CAP.5
Outpatient Versus Inpatient
Treatment
Most CAP patients
can be treated as outpatients.1 It is important to be certain that
the decision to admit to a hospital is the best choice, since the cost of
inpatient care can be up to 25 times that of an outpatient visit.16
Hospital admission can also increase the chances of the patient having
thromboembolic events or being infected by more virulent organisms.17
However, certain patients may need to be admitted to a hospital due to age,
comorbidities, and severity of the presenting disease. Severity of illness
scores, such as the CURB-65 criteria (Confusion, Uremia, R
espiratory rate, low Blood pressure, and age ?65), or
prognostic models such as the Pneumonia Severity Index (PSI) can be used to
help identify patients who may be better suited for outpatient therapy.5
It is important for a pharmacist to know whether a patient should be treated
in the outpatient setting or admitted to a hospital, as it will determine the
intensity of empiric antibiotic therapy, the amount of patient monitoring, and
the necessity of completing extra diagnostic testing.
Antibiotic Treatment
The goals of
pharmacotherapy for patients with CAP are to eliminate the causative organism,
resolve all clinical signs and symptoms, minimize hospitalization, and prevent
reinfection. Empiric antibiotic therapy is affected by expected CAP pathogens,
whether patients are admitted to a hospital or treated as outpatients, and the
presence of comorbidities. Table 3 indicates empiric treatment choices
for outpatients and inpatients with CAP.
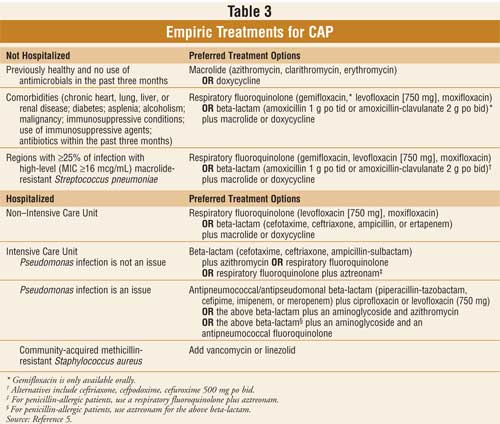
For empiric therapy, regardless of
admission or comorbidities, all patients should be treated with antibiotics
that are effective against S pneumoniae and atypical pathogens.18
If patients are ambulatory but have comorbidities, or if patients are at risk
for drug-resistant S pneumoniae (DRSP), more comprehensive antibiotic
therapy is required for them as compared with patients who are healthy and
ambulatory. If patients are hospitalized, antibiotic coverage becomes even
more aggressive and is provided initially in intravenous (IV) form. As the
level of severity of CAP increases, the potency of antibiotic therapy
increases. Pharmacists can assist physicians in choosing the most appropriate
empiric therapy based on the pharmacokinetic profile, expected adverse drug
reactions, cost-effectiveness, and previous drug exposure.
Drug-Resistant S
pneumoniae
Although
empiric pharmacotherapy is based upon the most likely pathogens to occur in
CAP, resistance patterns of pathogens to antibiotics can vary by geographic
region. The appearance of DRSP isolates is a well-documented phenomenon.5
DRSP can include resistance to beta-lactams, macrolides, and fluorquinolones.
The clinical significance of DRSP is not fully known.5 In many
cases, increasing the dosage of certain agents (i.e., penicillins,
cephalosporins, and the fluoroquinolone levofloxacin) will lead to an adequate
outcome in patients with DRSP.5 Despite the positive outcome, use
of these agents may not necessarily prevent the emergence of more drug
resistance. Switching to a more potent agent (gemifloxacin or moxifloxacin)
may provide the desired result and may lead to a stabilization or even a de
crease in resistance rates.19,20
Switching from Intravenous
to Oral Therapy
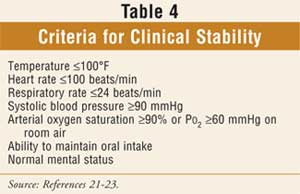
Patients may be
switched from IV to oral therapy when they are hemodynamically stable and have
improved clinically, when they are able to ingest oral medications, and when
they have a normal-functioning gastrointestinal tract.5 Table 4
indicates criteria that can be used to help define clinical stability.21
Currently, the use of potent antibiotics with high bioavailability allows
most patients who are able to eat and drink to switch to oral therapy. When
switching to an oral antibiotic, the same agent as the IV antibiotic or an
agent from the same class should be used.5 It is probably not
necessary to switch to a drug from a different class primarily due to its
higher bioavailability (e.g., the fluoroquinolones) in patients who are
responding.5 For those on a beta-lactam/macrolide combination,
changing to a macrolide alone appears to be adequate in patients who do not
have DRSP or who are infected with gram-negative enteric pathogens.24
Duration of Treatment
Patients with CAP
should be treated for a minimum of five days, should be afebrile for 48 to 72
hours, and should not have more than one CAP-associated criterion for clinical
instability (see Table 4). Formerly, most patients with CAP were
treated with seven to 10 days (or longer) of antibiotic therapy. Recent
studies have indicated that five days of therapy appears to be the minimum
period of time for typical CAP patients.25-27 A longer duration of
therapy may be needed if initial therapy was not active against the identified
pathogen or if it was complicated by extrapulmonary infections such as
meningitis or endocarditis.5
Monitoring CAP Therapy
The main goal in
the treatment of CAP is complete cure of the infection. A community pharmacist
can assist in this outcome by monitoring for both efficacy of the medication
prescribed and its particular toxicity. Most patients will become clinically
stable within three to seven days of appropriate antimicrobial therapy.5
During this period, pharmacists can ask patients if symptoms are resolving.
Questions include: Has fever resolved? Do you find it easier to breathe? Are
you coughing less? When you cough, does less material come up? It is important
for pharmacists to educate patients about expected and possible side effects,
as well as drug interactions.
Prevention of CAP
CAP, whether caused
by the influenza virus or by pneumococcal bacteria, can be prevented by
immunization. All persons ages 50 and older, people at risk for influenza
complications, and those with household contact with high-risk persons and
high-risk health care workers should receive the inactivated influenza vaccine
yearly.5 Pneumococcal polysaccharide vaccine is recommended for
those ages 65 and older and for those with high-risk concurrent diseases.5
The Role of the Pharmacist
Pharmacists can
assist in the prevention and treatment of this potentially life-threatening
infectious disease. Pharmacists can help identify those patients at risk for
developing CAP and can recommend immunization. When CAP occurs in a patient, a
pharmacist can work with the health care team to provide the most effective
therapy based on the patient's particular needs (e.g., cost considerations,
underlying comorbidities, possible drug interactions, and local bacterial
resistance patterns). Pharmacists can also aid in the monitoring of CAP
treatment by assessing the success of therapy with respect to resolution of
symptoms. Finally, effective counseling by the pharmacist can halp achieve
compliance and overall clinical cure. Effective counseling allows the patient
to truly understand all aspects of his or her drug therapy (e.g., side
effects, time to resolution of symptoms) and thus encourages full compliance.
References
1. Bartlett JG, Dowell SF, Mandell LA, et al; Infectious Diseases Society of America. Practice guidelines for the management of community-acquired pneumonia. Clin Infect Dis. 2000;31:347-382.
2. National Center for Health Statistics. Health, United States, 2006. Available at: www.cdc.gov/nchs/data/hus/hus06.pdf. Accessed June 6, 2007.3. DeFrances CJ, Podgornik MN. 2004 National hospital discharge survey. Adv Data. 2006;317:1-19.
4. Division of Epidemiology. National Heart Lung and Blood Institute. Morbidity and mortality: 2004 chartbook on cardiovascular, lung and blood diseases. May 2004.
5. Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27-S72.
6. Mandell GL, Bennett JE, Dolin R. Principles and Practice of Infectious Diseases. 6th ed. Philadelphia, PA: Churchill Livingstone; 2005:819-845.
7. Marrie TJ, Durant H, Yates L. Community-acquired pneumonia requiring hospitalization: 5-year prospective study. Rev Infect Dis. 1989;11:586-599.
8. Marrie TJ. Community-acquired pneumonia. Clin Infect Dis. 1994;18:501-513.
9. Paganin F, Lilienthal F, Bourdin A, et al. Severe community-acquired pneumonia: assessment of microbial aetiology as mortality factor. Eur Respir J. 2004;24:779-785.
10. Arancibia F, Bauer TT, Ewig S, et al. Community-acquired pneumonia due to gram-negative bacteria and Pseudomonas aeruginosa: incidence, risk, and prognosis. Arch Intern Med. 2002;162:1849-1858.
11. File TM. Community-acquired pneumonia. Lancet. 2003;362:1991-2001.
12. Halm EA, Teirstein AS. Clinical practice. Management of community-acquired pneumonia. N Engl J Med. 2002;347:2039-2045.
13. Metlay JP, Fine MJ, Schulz R, et al. Measuring symptomatic and functional recovery in patients with community-acquired pneumonia. J Gen Intern Med. 1997;12:423-430.
14. Metlay JP, Schulz R, Li YH, et al. Influence of age on symptoms at presentation in patients with community-acquired pneumonia. Arch Intern Med. 1997;157:1453-1459.
15. Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA. 1997;278:1440-1445.
16. Niederman MS, McCombs JS, Unger AN, et al.The cost of treating community-acquired pneumonia. Clin Ther. 1998;20:820-837.
17. Alikhan R, Cohen AT, Combe S, et al. Risk factors for venous thromboembolism in hospitalized patients with acute medical illness: analysis of the MEDENOX Study. Arch Intern Med. 2004;164:963-968.
18. Lieberman D, Schlaffer F, Boldur I, et al. Multiple pathogens in adult patients admitted with community-acquired pneumonia: a one year prospective study of 346 consecutive patients. Thorax . 1996;51:179-184.
19. Waterer GW, Buckingham SC, Kessler LA, et al. Decreasing b-lactam resistance in Pneumococci from the Memphis region: analysis of 2,152 isolates from 1996 to 2001. Chest. 2003;124:519-525.
20. Chen DK, McGeer A, de Azavedo JC, Low DE. Decreased susceptibility of Streptococcus pneumoniae to fluoroquinolones in Canada. Canadian Bacterial Surveillance Network. N Engl J Med. 1999;341:233-239.
21. Ramirez JA, Srinath L, Ahkee S, et al. Early switch from intravenous to oral cephalosporins in the treatment of hospitalized patients with community-acquired pneumonia. Arch Intern Med . 1995;155:1273-1276.
22. Halm EA, Fine MJ, Marrie TJ, et al. Time to clinical stability in patients hospitalized with community-acquired pneumonia: implications for practice guidelines. JAMA. 1998;279:1452-1457.
23. Menéndez R, Torres A, Rodríguez de Castro F, et al. Reaching stability in community-acquired pneumonia: the effects of the severity of disease, treatment, and the characteristics of patients. Clin Infect Dis. 2004;39:1783-1790.
24. Zervos M, Mandell LA, Vrooman PS, et al. Comparative efficacies and tolerabilities of intravenous azithromycin plus ceftriaxone and intravenous levofloxacin with step-down oral therapy for hospitalized patients with moderate to severe community-acquired pneumonia. Treat Respir Med. 2004;3:329-336.
25. Dunbar LM, Wunderink RG, Habib MP, et al. High-dose, short-course levofloxacin for community-acquired pneumonia: a new treatment paradigm. Clin Infect Dis. 2003;37:752-760.
26. Rizzato G, Montemurro L, Fraioli P, et al. Efficacy of a three day course of azithromycin in moderately severe community-acquired pneumonia. Eur Respir J. 1995;8:398-402.
27. Schonwald S, Skerk V, Petricevic I, et al.
Comparison of three-day and five-day courses of azithromycin in the treatment
of atypical pneumonia. Eur J Clin Microbiol Infect Dis. 1991;10:877-880.
To comment on this article, contact
editor@uspharmacist.com.





