US Pharm.
2008;33(5):28-30.
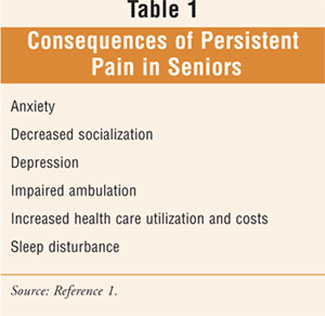
There are numerous consequences of persistent pain in older adults (TABLE 1
). The clinical manifestations of persistent pain cross physiologic,
psychologic, and social domains.1 Understanding these potential
consequences provides insight into the challenging task of formulating an
appropriate pharmaceutical care plan for individuals with this condition. The
greatest challenge usually involves the treatment of the oldest, sickest, and
most frail seniors with multiple comorbidities and few to no social supports.
1 Furthermore, some conditions may be worsened by the presence of pain,
including gait disturbances, slow rehabilitation, and adverse effects from
polypharmacy (e.g., nonsteroidal anti-inflammatory drug [NSAID]-induced acute
renal failure).1,2 Through the integration of information regarding
persistent pain with pharmacokinetic and pharmacodynamic principles associated
with drug utilization in the elderly, pharmacists involved in pain management
can become skillful in recommending medication regimens tailored to each
individual patient.
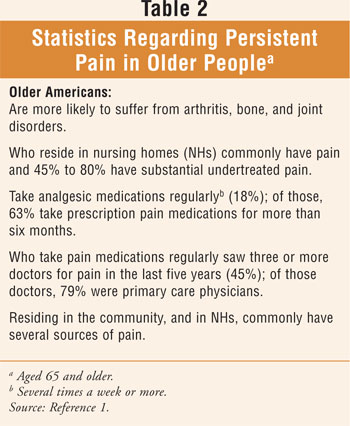
Persistent Pain
The most common reason patients seek out medical care is pain.3
Persistent pain, common among older Americans (TABLE 2), may be defined
as a painful experience that continues for a prolonged period of time and may
or may not be associated with a recognizable disease process, according to The
American Geriatrics Society Panel on Persistent Pain in Older Persons.1
The term chronic pain has been replaced with the preferred term
persistent pain in an attempt to remove negative connotations (e.g.
chronic psychiatric problems, malingering, drug-seeking behavior) and foster a
more positive attitude by those involved in the management of pain and
alleviation of suffering in the elderly (e.g., patients, caregivers, and
professionals).1 Patients with persistent pain can experience a
pain exacerbation, referred to as breakthrough pain, as well as acute
pain secondary to a new illness or condition.4,5
Consequences of Persistent Pain
Unlike acute pain that is often associated with hyperactivity of the
sympathetic nervous system (e.g., elevated blood pressure and respiratory
rate, tachycardia, diaphoresis, dilated pupils), persistent pain frequently
leads to gradually developing vegetative signs (e.g., listlessness, decreased
appetite, loss of taste for food, weight loss, decreased libido, constipation,
and sleep disturbance).3 Impaired ambulation may also be observed.
In the elderly, psychosocial factors both affect pain and are affected by pain.
1 Patients with persistent pain may withdraw socially; psychologic and
social impairment may be severe, resulting in virtual lack of function.3
Older adults with good coping strategies have been shown to have considerably
lower pain and psychologic disability.1 Depression may occur in
patients with persistent pain and is commonly associated with pain in the
elderly; a significant correlation has been shown between pain and depression
among nursing home residents.1,3 Untreated pain may manifest as
anxiety, refusal of care (i.e., physical assistance or handling of the patient
may exacerbate pain), and agitated behaviors.6,7 Patients may
become preoccupied with physical health, further contributing to the increased
health care utilization and costs resulting as a consequence of persistent
pain.
Pain Assessment
The patient's report is the most accurate and reliable evidence of the
existence of pain and its intensity; in most older people, a verbally
administered 0-10 scale is recommended to measure pain intensity.1
This concept has driven the phrase fifth vital sign, which refers to
pain and the need for its ongoing assessment. Ongoing assessment of pain
intensity is required to deliver quality of care since factors that exacerbate
pain and promote pain relief vary from patient to patient.7
Assessment may be especially challenging in older patients with dementia,
sensory impairments, and disability.1 Reference 8 contains an
example of a pain thermometer and faces scale that has been studied in the
elderly; a table of commonly identifiable pain-associated behaviors is also
available.8 It is important to note that an assessment should
include evaluation of acute pain that may indicate a new comorbidity
distinguishable from an exacerbation of persistent pain.1
Information obtained from caregivers and family members should be included in
the pain assessment.1
Minimum Data Set in Nursing
Homes
Consultant pharmacists who refer to the Minimum Data Set (MDS) 2.0 in the
medical records of nursing home and physical rehabilitation residents should
be aware of draft version MDS 3.0 containing changes involving pain assessment
items. These include: 1) treatment items added; 2) resident interview replaces
staff observations for residents who can report pain symptoms; 3) section
expanded to capture effect on function; 4) staff assessment of pain changed to
an observational checklist of pain behaviors and only completed for residents
who cannot self-report; and 5) a 10-point scale, providing a broader spectrum
of intensity and more broadly used in nursing homes and other settings, has
replaced the three-point scale. For a thorough review of the draft changes,
see Reference 9.
Management of Persistent Pain
Control of persistent pain involves analgesic medication dosed on a regular,
round-the-clock basis to avoid anxiety associated with the anticipation of
pain. Relieving breakthrough pain, escalating pain, or an exacerbation of a
preexisting morbidity that may contribute to the underlying pain requires a
rescue, as-needed analgesic medication order in addition to the scheduled
analgesic. Close monitoring of the frequency of use of rescue analgesics is
required for ongoing pain assessment; this enables the clinician to
recalculate an appropriate and adequate round-the-clock dosage regimen for the
relief of persistent pain. Cognitively intact patients may participate in
their treatment by using patient-controlled analgesia prescribed by their
physician.10
Adjuvant analgesic drugs, including anticonvulsants (e.g., carbamazepine,
valproate, gabapentin) and antidepressants (e.g., tricyclics [TCAs]),
venlafaxine, bupropion), are often utilized.3 These agents are used
for a variety of indications (both FDA-approved and off label); however, they
most notably target neuropathic pain. Gabapentin is the most widely prescribed
for this use.3 In the elderly: 1) TCAs (i.e., especially
amitriptyline, imipramine, and doxepin) can be problematic with regard to
anticholinergic and cardiac adverse effects; 2) gabapentin has been shown to
have decreased clearance as age increases--most likely due to age-related
decreases in renal function--and dose reductions may be necessary; and 3)
NSAIDs have the potential to produce gastrointestinal bleeding, renal failure,
high blood pressure, and heart failure.11 Topical medications such
as capsaicin (e.g., cream, lotion), compounded creams (e.g., local anesthetics
and NSAIDs), and a lidocaine 5% patch have low risk of side effects and should
be considered for various types of pain.3 Pharmacists, through
identifying, resolving, and preventing adverse effects of medications (e.g.,
constipation, excessive sedation, which may lead to respiratory depression),
are an integral part of the overall pain managementÜapproach.12
It has been suggested that in order to achieve comprehensive pain management,
it is important to relieve and prevent both the physical and emotional
symptoms.3,7,13,14 If depression is comorbid with persistent pain,
it should be treated with antidepressants.3 Psychologic and
behavioral treatments are usually helpful.3 Behavioral treatments
are capable of improving patient function, even without reducing pain.3
Pain control through cognitive techniques (e.g., biofeedback, hypnosis,
relaxation training, distraction techniques [guided imagery]) may be useful.
3
Physical therapy or occupational therapy may be beneficial in many patients;
some require an orthosis.3 Myofacial trigger points can be relieved
by spray-and-stretch techniques.3 Other treatments, depending on
the condition, include joint and spinal injections, trigger point injection,
nerve blocks, spinal cord stimulation, and neuraxial infusion.3
Future Trend in Persistent Pain Management
The treatment of persistent pain in the future appears to be evolving. Instead
of the current modalities providing symptomatic relief (e.g., morphine), newer
agents will aim at the disease process.15 Pain-sensing neurons of
the peripheral nervous system express several sodium channel subtypes, and
pharmacologic agents that target the Na 1.8 selective small molecule sodium
channel (subtype selective sodium channel blockers) are currently in
development.15
Conclusion
Clinical manifestations of persistent pain are usually multifactorial.
Pharmacists should develop an understanding of the nature of persistent pain
with regard to its consequences and ultimate potential to cause physical
impairment, psychologic disability, and social withdrawal. By integrating this
knowledge with appropriate pharmaceutical recommendations and ongoing pain
assessment, individualized medication regimens for persistent pain may be
achieved.
REFERENCES
1. The management of persistent pain in older persons. American Geriatrics
Society (AGS) Panel on Persistent Pain in Older Adults. 2002.
www.americangeriatrics.org/products/positionpapers/JGS5071.pdf. Accessed April
9, 2008.
2. Zagaria ME. Drug-induced acute renal failure: nonsteroidal
anti-inflammatory drugs. US Pharm. 2003;28(5):19-23.
www.uspharmacist.com/oldformat.asp?url=publish/content/8_1069.htm. Accessed
April 9, 2008.
3. Beers MH, Porter RS, eds. The Merck Manual of Diagnosis and Therapy.
18th ed. Whitehouse Station, NJ: Merck & Co.; 2006:1769-1779.
4. Burton AW. Outpatient management of breakthrough pain. Medscape Neurology &
Neurosurgery. 2005;7:1-6. www.medscape.com/viewarticle/506124. Accessed April
10, 2008.
5. Portenoy RK, Hagen NA. Breakthrough pain: definition, prevalence and
characteristics. Pain. 1990;41:273-281.
6. Martin CM. Understanding palliative care. The Consultant Pharmacist.
2006;21:698-713.
7. Zagaria ME. Geriatric palliative care: when the focus shifts from care to
comfort. US Pharm. 2007;32(5):28-34.
8. Zagaria ME. Pain assessment in older adults: the cornerstone of controlling
pain. US Pharm. 2006;31(5):30-36.
www.uspharmacist.com/oldformat.asp?url=publish/content/8_1735.htm. Accessed
April 9, 2008.
9. The MDS 3.0. Special Open Door Forum. January 24, 2008.
www.cms.hhs.gov/OpenDoorForums/Downloads/MDS30Word012408.pdf. Accessed April
11, 2008.
10. Lorenz K, Lynn J. Care of the dying patient. In: Hazzard WR, Blass JP,
Halter JB, et al. Principles of Geriatric Medicine and Gerontology. 5th
ed. New York: McGraw-Hill, Inc.; 2003:323-334.
11. Semla TP, Beizer JL, Higbee MD. Geriatric Dosage Handbook. 12th ed.
Hudson, OH: Lexi-Comp, Inc.; 2007.
12. ASHP 2006: Highlights of the 2006 American Society of Health-System
Pharmacists Midyear Clinical Meeting. Methadone, Pain Management, and
Palliative Care. www.medscape.com/viewarticle/550895. Accessed April 10, 2008.
13. Cohen AB, Koenig HG. Spirituality in palliative care. Geriatric Times.
2002;Nov/Dec:25.
14. Steinhauser KE, Clipp EC, Tulsky JA. Evolution in measuring the quality of
dying. J Palliat Med. 2002;5:407-414.
15. An Overview of the Decade of Pain Lecture From AAPM 2008: An Expert
Interview With Joshua P. Prager, MD, MS. Medscape Neurology & Neurosurgery.
2008; www.medscape.com/ viewarticle/570384. Accessed April 10, 2008.
To comment on this article, contact
rdavidson@jobson.com.





