US Pharm.
2008;33(12):20-22.
Visualizing organs of the
gastrointestinal (GI) tract, such as the liver and gallbladder, and detecting
cysts, abscesses, tumors, and obstructions can be achieved through
radiographic imaging.1 Contrast agents, used during a computed
tomography procedure, for example, can illuminate specific hollow structures
and vascularity of the GI tract.1 A coronary angiography, also
known as cardiac catheterization, can detect blockages through radiographic
visualization of coronary vessels subsequent to an injection of radiopaque
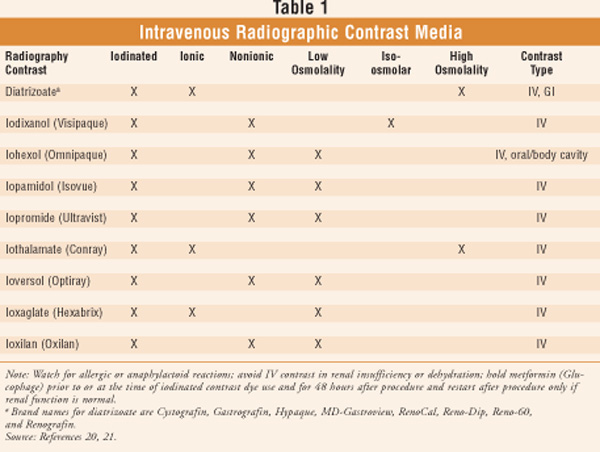
contrast medium (CM).2,3 Iodinated contrast media (TABLE 1),
used for the identification of vascular structures, are relied upon
continually in radiologic and cardiologic procedures.4
Contrast-induced nephropathy (CIN) is an increasingly important complication
associated with the use of iodinated CM.4
Diagnostic imaging procedures
that require intravenous radiographic CM have increased in number and
have resulted in an increase in CIN.5 CIN is considered a common
complication in angiographic procedures.6,7 This is an important
issue for clinicians, including pharmacists who provide services for the
elderly, since among aging individuals there is an increased incidence of
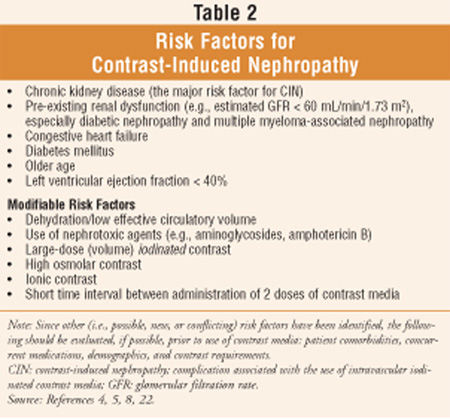
renal impairment and diabetes, two of the risk factors (TABLE 2) for
CIN.8,9 CIN is one of the most serious adverse events associated
with the use of CM and is the third leading cause of hospital-acquired acute
renal failure.10,11 It has been reported that individuals who
develop CIN have increased morbidity, higher rates of mortality, lengthy
hospital stays, and poor long-term outcomes.10 Choosing a
particular CM is dependent upon patient and procedural factors, current
evidence, and guidelines.8 Researchers indicate that chances of
developing CIN can be reduced by employing appropriate prevention strategies.10
Common Definitions of
Contrast-Induced Nephropathy
While the incidence
of CIN has been reported to vary widely, the true incidence of this condition
has been difficult to determine since there is no single definition of CIN.8,12
The most common definition of CIN used in clinical trials is: Increase in
baseline serum creatinine (SCr) of 0.5 mg/dL or 25% increase from baseline at
48 hours post CM usage.8,13 Other definitions include: Increase
in baseline SCr of > 0.5 mg/dL or > 25% within 72 hours post CM usage
excluding alternative reasons and Increase in baseline SCr of† >=
0.3 mg/dL, or an increase in SCr 50%, or oliguria (< 0.5 mL/kg/hour for > 6
hours).8,14,15 When CIN is suspected, other causes of renal
insufficiency should be considered in the differential diagnosis, such as
dehydration, interstitial nephritis, and cholesterol embolism.8
Pathophysiology
While changes in
the function of the aging kidney are highly variable and not always
inevitable, a decline in glomerular filtration rate (GFR)is masked in seniors
since a proportional decline in muscle mass renders the serum creatinine to
remain generally constant.16 When this consideration is not
acknowledged, it may result in inappropriate dosing of medications with
associated morbidity.16 Since even a subtle increase in serum
creatinine in seniors can signify a significant decline in renal function,
renal pathology may not be immediately recognized in a geriatric patient.16
The pathophysiology of
nephropathy secondary to contrast media is complex since its development is
multifactorial.8 A recent literature review proposed a simplified
sequence of events: When contrast media is administered in a subject with
impaired renal function (estimated GFR < 60 mL/min/1.73 m2), an
initial increase in renal blood flow occurs due to vasoconstrictors (e.g.,
endothelin, adenosine); this is followed by a decrease in blood flow, which
allows the contrast media to be pointedly nephrotoxic.8,13,17
Additionally, with the compromise of nitric oxide (a protective vasodilator)
production and the potential release of reactive oxygen species, further renal
injury may ensue.8,17-19 Research continues to identify patients at
risk for and measures to prevent CIN.8
Factors Increasing Risk
In an attempt to
reduce the chance of CIN, risk factors (TABLE 2) should be identified.
Among others, they include chronic kidney disease, older age, dehydration,
diabetes mellitus, congestive heart failure, and use of concurrent nephrotoxic
medication (including aminoglycosides and amphotericin B).5,10
CM Drug Interaction with
Metformin
Contrast agents may
increase the risk of metformin-induced lactic acidosis. Additionally, due to
the potential for acute alteration in renal function, metformin should be
temporarily discontinued for 48 hours in patients undergoing radiologic
studies involving IV administration of iodinated contrast media.20 Glucophage
should be restarted after the procedure only if renal function is normal.21
Measures for Prevention of
CIN
Currently, there is
no effective treatment for CIN.12 Researchers have noted that
although risk factors for CIN have been identified, an effective prophylaxis
strategy has not been developed for CIN due to a poor understanding of the
pathophysiology and the clinical significance of this condition.22
Among the categories of
developed strategies for the prevention of CIN (i.e., volume expansion before,
during, and after contrast media administration; pharmacological strategies to
prevent reduction of renal perfusion, reduction of tubular flow, and direct
tubular toxicity; renal replacement therapy; and selection of contrast media),
volume expansion is the most critical measure for reducing CIN and should be
used in all individuals undergoing procedures requiring CM.12
Research has revealed a general consensus that hydration protocols implemented
before and after imaging with CM may prevent CIN.9 Unfortunately,
definitive and convincing data have not established amounts to be infused,
infusion timing, and type of solutions (i.e., half-isotonic, isotonic saline
solution, or bicarbonate).9 An extensive Medline search indicates
it is believed that prevention is actually achieved through the correction of
hypovolemia, dehydration, or both.9 In addition to the utilization
of hydration, use of low volumes of iso-osmolar or low-osmolar contrast in
those patients at risk of developing CIN has been recommended.6,22
While the use of
N-acetylcysteine or ascorbic acid has been suggested as possibly valuable in
very high-risk patients, no consensus exists to date regarding the efficacy of
N-acetylcysteine for CIN prevention.8,22 Randomized trials have
provided evidence that interventions such as theophylline, bicarbonate, and
ascorbic acid were appropriate in the emergency department setting and did
decrease the risk of CIN.11
The recommendation to obtain
serum creatinine levels prior to the procedure among patients with renal
disease, diabetes, proteinuria, hypertension, gout, or congestive heart
failure is supported by practice guidelines.22 While beyond the
scope of this article, a list of organizational guidelines and recommendations
regarding the prevention and monitoring of CIN, including the American College
of Radiology and two consensus panels, can be found in Reference 8.
Researchers have called for future research to focus on correctly identifying
higher risk patients and studying therapies as part of large, well-designed
clinical trials.7,22
Conclusion
The wide use of
diagnostic imaging with IV iodinated CM places an ever increasing number of
patients in contact with a renally toxic agent with potential for adverse
outcomes, especially those at risk, such as geriatric patients. CIN is
associated with significant economic and clinical consequences, including
prolonged hospitalization and a higher rate of mortality. While it is believed
that prevention is actually achieved through the correction of hypovolemia,
dehydration, or both, further research involving large clinical trials is
warranted to test and develop prevention protocols.
REFERENCES
1. Chisholm MA,
Jackson MW. Evaluation of the gastrointestinal tract. In: DiPiro JT, Talbert
RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach.
6th ed. New York, NY: McGraw-Hill, Inc; 2005:605-612.
2. Talbert RL.
Cardiovascular testing. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy:
A Pathophysiologic Approach. 6th ed. New York, NY: McGraw-Hill, Inc;
2005:149-170.
3. Beers MH, Jones TV,
Berkwits M, et al, eds. The Merck Manual of Health & Aging.
Whitehouse Station, NJ: Merck Research Laboratories; 2004:104-123.
4. McCullough PA. CIN
Consensus Working Panel: Executive Summary.
www.c2i2.org/vol_v_issue_1/cin_consensus_working_panel.asp.
Accessed November 11,
2008.
5. van den Berk G,
Tonino S, de Fijter C, et al. Bench-to-bedside review: preventive measures for
contrast-induced nephropathy in critically ill patients. Crit Care.
2005;9:361-370. Epub 2005 Jan 7.
6. Pannu N, Tonelli M.
Strategies to reduce the risk of contrast nephropathy: an evidence-based
approach. Curr Opin Nephrol Hypertens. 2006;15:285-290.
7. Zagler A, Azadpour
M, Mercado C, et al. N-acetylcysteine and contrast-induced nephropathy: a
meta-analysis of 13 randomized trials. Am Heart J. 2006;151:140-145.
8. Contrast Media
Reactions Pose Serious Risk of Nephropathy. Medscape Pharmacists. 2008.
www.medscape.com/viewarticle/577203?src=mp&spon=30&uac=7376SZ.
Accessed November 5, 2008.
9. Meschi M, Detrenis
S, Musini S, et al. Facts and fallacies concerning the prevention of contrast
medium-induced nephropathy. Crit Care Med. 2006;34:2060-2068.
10. Stacul F. Reducing
the risks for contrast-induced nephropathy. Cardiovasc Intervent Radiol.
2005;28(suppl 2):S12-S18.
11. Sinert R, Doty CI.
Evidence-based emergency medicine review. Prevention of contrast-induced
nephropathy in the emergency department. Ann Emerg Med.
2007;50:335-345, 345.e1-2. Epub 2007 May 21.
12. Feldkamp T, Kribben
A. Contrast media induced nephropathy: definition, incidence, outcome,
pathophysiology, risk factors and prevention. Minerva Med.
2008;99:177-196.
13. McCullough PA.
Contrast-induced acute kidney injury. J Am Coll Cardiol.
2008;51:1419-1428.
14. Thomsen HS, Morcos
SK. Contrast media and the kidney: European Society of Urogenital Radiology
(ESUR) guidelines. Br J Radiol. 2003;76:513-518.
15. Mehta RL, Kellum
JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to
improve outcomes in acute kidney injury. Crit Care. 2007;11:R31.
16. Bailey JL, Sands
JM. Renal disease. In: Hazzard WR, Blass JP, Halter JB, et al, eds. Principles
of Geriatric Medicine and Gerontology. 5th ed. New York, NY: McGraw-Hill,
Inc; 2003:551-568.
17. Bartorelli AL,
Marenzi G. Contrast-induced nephropathy. J Interv Cardiol.
2008;21:74-85.
18. Tumlin J, Stacul F,
Adam A, et al. Pathophysiology of contrast-induced nephropathy. Am J
Cardiol. 2006;98:14K-20K.
19. Persson PB, Tepel
M. Contrast medium-induced nephropathy: the pathophysiology. Kidney Int.
2006;69:S8-S10.
20. Semla TP, Beizer
JL, Higbee MD. Geriatric Dosage Handbook. 12th ed. Hudson, OH:
Lexi-Comp, Inc; 2007.
21. Radiography
contrast. Tarascon Pocket Pharmacopeia. Redlands, CA: Tarascon
Publishing; 2008:53.
22. Pannu N, Wiebe N,
Tonelli M; Alberta Kidney Disease Network. Prophylaxis strategies for
contrast-induced nephropathy. JAMA. 2006;295:2765-2779.
To comment on this article, contact
rdavidson@jobson.com.





