US
Pharm.
2006;1:HS-14-HS-22.
Fibromyalgia syndrome (FMS) is
a chronic, soft-tissue pain disorder that affects about 3.7 million people in
United States, the majority (75%) of whom are women.1 The condition
is characterized by fatigue and widespread pain in muscles, ligaments, and
tendons and is a common cause of chronic musculoskeletal pain. Patients with
FMS often report tender point pain that occurs in local sites --usually in the
neck and shoulders--and radiates out into other regions of the body. Such pain
can occur in areas where the muscles attach to bone or ligaments, but the
joints are not affected. Pain resulting from FMS is similar to that of
arthritis and has been described as stiffness, burning, radiating, and aching.
The generalized pain of FMS is often
accompanied by many other symptoms, including depression, headache,
paresthesias, fatigue, poor sleep, and morning stiffness (Table 1). As more
attention is given to the pharmacological treatment of this disorder,
pharmacists will likely receive questions from patients with FMS. This article
will help pharmacists to effectively counsel patients with fibromyalgia and
recognize patients with FMS-like symptoms who are self-treating, since some of
these patients may need medical treatment.

Epidemiology
The exact etiology and
pathogenesis of FMS is essentially unknown. Due to its similarity to other
disease states and lack of objective symptoms, the disorder is often difficult
to diagnose. FMS affects about 2% to 3% of the general population and more
than 5% of patients in general medical practice.1,2 The typical age
of patients with FMS ranges from mid-30s to late-50s. One study found that
generalized musculoskeletal pain in women was increasingly prevalent as age
increased from 18 to 70 years.3 Patients often report that their
pain is continuous and can vary depending on time of day, weather changes,
physical activity, and the presence of stressful situations. Insomnia often
exacerbates the pain.
Pathophysiology
Multiple
physiologic alterations such as sleep disturbances, altered neurotransmitter
metabolism, and muscle structure abnormalities have been proposed to account
for the symptoms associated with FMS. Such theories involving sleep and
neurotransmitter alterations are widely accepted. Poor sleeping patterns are
very prevalent in patients with FMS and can affect their stress response
system. This contributes to negative mood, cognitive difficulties, and
increased pain perception.4-6 The stress response may become
maladaptive in chronic pain syndromes and contribute to symptoms such as
fatigue, poor sleep, low mood and/or anxiety, and "flu-like" illness.
4 Evidence suggests that psychological stress can initiate alterations
of the stress response system, with multiple adverse effects on the
neuroendocrine, immunologic, and autonomic nervous systems.5,6
Decreases in serum serotonin, which modulates pain and stage 4 sleep, have
also been noted. In addition, levels of serotonin's precursor, tryptophan, may
be low in patients with FMS.5 The theory that altered serotonin may
be involved in the pathogenesis of FMS has led to the use of selective
serotonin reuptake inhibitors (SSRIs) for treatment. Other biochemical
abnormalities include an elevated level of substance P in cerebral spinal
fluid (80% of patients).7 Hyaluronic acid levels are high early in
the day, and changes in serum levels are related to the intensity of morning
stiffness.7
The simultaneous processing of
sensory and emotional aspects of pain may influence the subjective intensity
of FMS symptoms. Patients with FMS have distorted central nociceptive
processing, which alters the pain perception and pain tolerance thresholds.
The two principal effectors of the stress response, the hypothalamic pituitary
axis and the sympathetic nervous system, are activated in pain states.6
Negative emotions and psychological factors can heighten the pain experience
and pain-processing systems. The four principal categories of pain are (1)
nociceptive pain (matches the noxious stimulus), (2) neuropathic pain (may
follow injuries/diseases that directly affect the nervous system), (3)
psychogenic pain (occurs in disorders associated with psychological factors),
and (4) complex pain of complex etiology (occurs in fibromyalgia). The number
of painful tender points is strongly correlated with psychological distress in
patients with FMS (table 2).

Aggravating Factors in FMS
Fibromyalgia is a
chronic illness whose outcomes are influenced by the interaction of
biological, psychological, and sociological factors.8 Important
biological factors include gender, sleep, physical condition, neuroendocrine
and autonomic dysregulation, and sensitization to pain. Female gender is
associated with increased pain sensitivity. Clinical studies have shown that
females have more pain, use analgesics more often, and are influenced by
fluctuations in hormone levels.9 Stress and noxious stimuli are
more likely to trigger a response in females than in males. Compared with men,
women report more symptoms, including unexplained symptoms.9,10
Other variables such as environment and ethnicity can influence the course of
pain and fatigue. Cognitive factors in the pain and fatigue associated with
FMS include hypervigilance, management strategies, perceived pain control,
mood, depression, anxiety, and personal behaviors. Psychosocial factors such
as poor health of parents, poor family environment, and childhood
abuse--particularly sexual abuse--may influence a patient's vulnerability or
susceptibility to FMS. The disorder often has a high impact on the patient,
the patient's family, and society. Physical functioning, emotional well-being,
social functioning, and general health perception all contribute to the
patient's quality of life. In approximately one half of cases, symptoms of FMS
appeared to begin after a specific event, most often some form of physical or
emotional trauma.11
Typical Clinical
Presentation of FMS
The chief complaint
of patients with FMS is diffuse musculoskeletal pain. Several characteristics
and painful "trigger points" are associated with FMS (tables 1, 2
). Although initially the pain may be localized, it can spread to many muscle
groups. Patients typically complain of pain in the neck, back, chest wall,
arms, and legs. The pain is recurring and fluctuates in intensity. Sensations
of tingling and burning are often described. Patients with FMS may have a
variety of symptoms that are not well understood, including abdominal pain
suggestive of irritable bowel syndrome and bladder symptoms indicative of
interstitial cystitis. Fatigue is one of the most common complaints. Most
patients report light sleep and/or feeling groggy in the morning. Mood
disturbances, short-term memory loss, headaches, and feeling faint and/or
dizzy are also frequent complaints. Less common symptoms include ocular
dryness, dysphagia, palpitations, dyspnea, dysmenorrhea, osteoporosis, weight
fluctuations, allergic symptoms, and night sweats. Typically, the only helpful
finding on physical exam is excessive tenderness. The rest of the exam is
usually only helpful to rule out other conditions. Patients often have
difficulty distinguishing joint and muscle pain and may complain of swelling,
although the joints do not appear inflamed on exam. There is no evidence to
indicate a connective tissue disorder unless the patient has an associated
illness. FMS may occur with any rheumatic disorder.12
FMS frequently exists with
other illness. In one study, 22% of patients with systemic lupus erythematosus
met the American College of Rheumatology criteria for fibromyalgia.10
Coexisting connective tissue diseases, psychiatric illnesses, sleep
disorders, and chronic infections complicate the assessment and diagnosis of
FMS because of the similarities in symptoms. Approximately 30% of patients
with FMS have major mood disorders.13 A change in affect is often
the patient's primary complaint.14 The combination of poor
sleep, fatigue, and widespread pain is observed in disorders such as restless
legs syndrome and sleep apnea. Pain and tenderness are also present in some
patients who have an infectious disease. FMS overlaps with other poorly
understood syndromes. Patients with chronic fatigue syndrome often meet tender
point criteria for FMS. Myofascial pain can also complicate assessment and
diagnosis. Patients with chronic fatigue syndrome often complain of localized
pain, and some consider it to be a localized form of FMS.15
Overview of Treatment of FMS
The classification
and diagnosis of FMS is a critical step in improving a patient's quality of
life. The goal of FMS therapy is palliation of symptoms, since there is no
curative treatment of FMS and remission of all symptoms is rarely achieved.
Since there is no consensus on effective pharmacological treatment for FMS,
most patients are treated symptomatically for pain, insomnia, underlying
depression, and muscle tension.
Treatment is multifaceted and includes
patient education, pharmacotherapy, physical and occupational therapy, and
occasionally behavioral or psychotherapy. A treatment program that
incorporates physicians, rehabilitation, and mental health specialists will
likely be more successful than drug treatment alone.16 Results of
educational interventions alone are often superior to those in control groups,
with respect to pain relief.16 Educational interventions should
explain the nature of FMS and provide a rationale for the treatment program. A
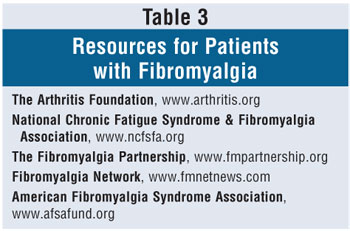
list of resources for patients with FMS can be found in Table 3. Patients
should have an active role in the treatment plan, understand the role of
stress, and learn techniques that can reduce it.
Pharmacotherapy
SSRIs and tricyclic
antidepressants have proven to be somewhat effective. In one study, fluoxetine
was superior to placebo at reducing pain and change in mood.17
Doses of up to 80 mg of fluoxetine per day were used in 60 women (ages 21 to
71 years) with FMS. Patients were randomly assigned to receive fluoxetine (10
to 80 mg/day) or placebo for 12 weeks in a double-blind,
parallel-group, flexible-dose study. Women who received fluoxetine (mean dose,
45 mg/day) had a significant (P = .005) improvement of the Fibromyalgia
Impact Questionnaire (FIQ) total score, compared with women who received
placebo. The FIQ is a self-reported survey of 19 items that measure physical
functioning and intensity of symptoms. The fluoxetine group also showed
significant improvement of their pain (P = .002), fatigue (P =
.05) and depression (P = .01) scores, compared with women who received
placebo. The number of tender points and total myalgic scores improved more in
the fluoxetine group than in the placebo group, but these differences were not
statistically significant. Fluoxetine was generally well tolerated.
A meta-analysis of clinical
trials using antidepressants for the treatment of FMS shows that these drugs
have only modest efficacy in treating many of the symptoms of fibromyalgia.
18 Sixteen randomized placebo-controlled trials were identified, of
which 13 were appropriate for data extraction. There were three classes of
antidepressants evaluated: tricyclics (nine trials), SSRIs (three trials), and
S-adenosylmethionine (two trials). Patients were more than four times as
likely to report overall improvement and reported moderate reductions in
individual symptoms, particularly pain. It is uncertain whether this effect is
independent of depression. Doses lower than those required for depression
should be used at bedtime (e.g., nortriptyline 25 to 50 mg at bedtime).
However, the adverse side effects of some of these drugs may limit their use,
especially the highly anticholinergic drug amitriptyline.
A number of medications,
including analgesic, anti-inflammatory, and central nervous system (CNS) drugs
have been used in the treatment of FMS. In 2003, a study assessed the efficacy
of acetaminophen and tramadol in patients with fibromyalgia.19 The
purpose of the study was to evaluate the efficacy and safety of a combination
analgesic tablet (37.5 mg tramadol/325 mg acetaminophen) for the treatment of
fibromyalgia pain. The 91-day, multicenter, double-blind, randomized,
placebo-controlled study compared tramadol/acetaminophen combination tablets
with placebo. The primary outcome variable was cumulative time to
discontinuation (Kaplan-Meier analysis). Secondary measures at the end of the
study included pain, pain relief, total tender points, myalgia, health status,
and FIQ scores. There were 315 subjects enrolled in the study, 94% female.
Tramadol/acetaminophen–treated subjects had significantly less pain at the end
of the study, better pain relief, and better FIQ scores (all statistically
significant). Indexes of physical functioning, role-physical, body pain,
health transition, and physical component summary improved significantly in
subjects receiving the tramadol/acetaminophen tablets. Discontinuation due to
adverse events occurred in 19% (n = 29) of tramadol/acetaminophen–treated
subjects and 12% (n = 18) of placebo-treated subjects. Patients who had
experienced treatment failure on other medications were excluded. In addition,
tramadol as a weak mu-receptor agonist has some abuse potential and should be
prescribed with caution.
In a study of 58 females with
fibromyalgia, 74.1% completed an eight-week treatment period testing the
combination of carisoprodol, acetaminophen, and caffeine versus placebo.20
Twenty-three patients received placebo and 20 received active medication. In
the placebo group, 56.5% of patients used additional analgesics, compared to
only 20% in the active treatment group (P = .015). Forty-three percent
of patients in the placebo group and none of the patients in the active
treatment group used tricyclic antidepressants, anxiolytics, or sedatives (P
= .0008). Patients receiving active medication reported statistically
significant improvement for pain (P <.01), sleep quality (P
<.01) and a general feeling of sickness (P <.05). An increased
pressure pain threshold was found in the active treatment group after eight
weeks in 70% of the sites measured, while the pressure pain threshold
increased in only 30% of the sites in the placebo group. The authors concluded
that the combination of carisoprodol, acetaminophen, and caffeine is effective
in the treatment of fibromyalgia. However, the study's small sample size
should be considered.
A randomized crossover trial
studied the use of fluoxetine and amitriptyline together.21 This
combination provided better results than either drug alone. The use of a drug
or combination of drugs that inhibit reuptake of both serotonin and
norepinephrine may be more useful than a drug that targets only one
neurotransmitter. Duloxetine and venlafaxine are two drugs that inhibit
reuptake of both neurotransmitters and may be useful in the treatment of FMS.
Pregabalin is an alpha-2 delta
ligand being studied for chronic pain and epilepsy. A recent trial was
conducted to evaluate the efficacy and safety of pregabalin for treatment of
symptoms associated with FMS.22 The multicenter, double-blind,
eight-week, randomized study measured the effect of pregabalin doses of 150,
300, and 450 mg/day on pain, sleep, fatigue, and health-related quality of
life in patients with FMS (n = 529) against placebo. The primary outcome was
the comparison of mean end-point pain scores, derived from daily diary ratings
of pain intensity from the pregabalin treatment groups and the placebo group.
Pregabalin at 450 mg/day significantly reduced the average severity of pain in
the primary analysis compared with placebo. Significantly more patients
treated with pregabalin had improvement in pain at the end point (29% vs. 13%
in the placebo group; P = .003). Pregabalin at 300 and 450 mg/day was
associated with significant improvements in sleep quality, fatigue, and global
measures of change. Dizziness and somnolence were the most frequently reported
adverse effects. Rates of discontinuation due to adverse events were similar
across all treatment and placebo groups. The authors concluded that pregabalin
at 450 mg/day was well tolerated and effective to treat FMS compared with
placebo, resulting in reduced symptoms of pain, disturbed sleep, and fatigue.
Duloxetine was studied in 207
patients with primary fibromyalgia, with or without current major depressive
disorder.23 The study was a randomized, double-blind,
placebo-controlled trial conducted in 18 outpatient research centers in the
U.S. Subject charcteristics were as follows: 89% female, 87% white, mean age
of 49 years, and 38% with a current major depressive disorder. After a
single-blind placebo treatment for one week, subjects were randomly assigned
to receive duloxetine 60 mg twice a day or placebo for 12 weeks. Compared with
placebo, duloxetine-treated subjects showed significantly greater improvement
of pain, fibromyalgia, and quality of life. Duloxetine treatment improved
fibromyalgia symptoms and severity of pain regardless of baseline status of
depression. Compared with placebo-treated females, duloxetine-treated females
showed greater improvement on most efficacy measures, while duloxetine-treated
male subjects failed to improve significantly. However, it is important to
note that there were far fewer male subjects in the study. In females, the
effect of treatment on pain reduction was independent of the effect on mood or
anxiety. Duloxetine was well tolerated, with adverse effects being similar to
those reported with placebo.
Cyclobenzaprine has been shown
to be mildly effective in a meta-analysis of placebo-controlled trials.24
The meta-analysis showed that when patients are treated with cyclobenzaprine,
they are three times as likely to report an improvement in pain. Five patients
would need to be treated with the drug in order for one to improve. According
to this analysis, generalized pain improved early on with the drug, but there
was no improvement in fatigue or tender points at any time. Using a variety of
outcome measures, cyclobenzaprine-treated patients were three times as likely
to report overall improvement and moderate reductions in individual symptoms,
particularly sleep. A 5- to 10-mg dose three times daily was used. Patients
should be warned of prominent CNS side effects with cyclobenzaprine, including
dizziness, sedation, and dry mouth.
There are a number of
nonmedicinal options that may be effective for the treatment of fibromyalgia.
FMS patients typically avoid exercise because they believe that their pain
worsens after exercise. Aerobic activities such as biking, swimming, and
running are sometimes successful in attenuating FMS symptoms. In controlled
trials, aerobic exercise was able to decrease the amount of pain reported and
increased the threshold for pain.25,26 Strength training using
weights and elastic bands has been effective in reducing pain and the number
of tender points.26 Complementary and alternative medicine (CAM) is
sometimes used by FMS patients. However, evidence to confirm its
effectiveness is limited. It is important that the physician and pharmacist be
aware of all CAM substances the patient is taking, since some may have drug
interactions with prescribed therapy.
Some studies have shown that S
-adenosylmethionine can reduce pain and improve quality of sleep and sense of
well-being, while other studies have shown no benefit.27,28 In
addition, 5-hydroxytryptophan (5-HTP), the precursor to serotonin, has been
shown to have some benefit in FMS patients.29 Oral doses of 5-HTP
100 mg three times daily improved pain severity, quality of sleep, anxiety,
and the number of tender points. Additional options include hypnotherapy,
meditation, and cognitive behavioral therapy.30,31 These options
have shown some usefulness in selected FMS patients.
Pharmacist-to-Patient Counseling
Pharmacists should
reassure patients with FMS that improvement in pain tolerance, sleep, and
fatigue is likely with appropriate comprehensive and multidisciplinary
treatment. However, patients should understand that there is no cure for FMS,
and complete pain relief is often not possible. Pharmacists should emphasize
that active patient participation in the treatment program can help reduce
symptoms and improve quality of life. Patients should be educated about the
possible causes and aggravating factors of FMS.
REFERENCES
1. Wolfe F, Cathey
MA. Prevalence of primary and secondary fibrositis. J Rheumatol.
1983;10(6):965-968.
2. Campbell SM, Clark
S, Tindall EA, et al. Clinical characteristics of fibrositis: a blinded
controlled study of symptoms and tender points. Arthritis Rheum.
1983;26:817-824.
3. Wolfe F, Smythe HA,
Yunus MB, et al. The American College of Rheumatology 1990 criteria for the
classification of fibromyalgia: Report of the multicenter criteria committee.
Arthritis Rheum. 1990;33:160-172.
4. Goldenberg DL.
Fibromyalgia, chronic fatigue syndrome, and myofascial pain syndrome. Curr
Opin Rheumatol. 1994;6:223-233.
5. Russell IJ.
Neurochemical pathogenesis of fibromyalgia syndrome. J Musculoskel
Pain. 1996;4:61-92.
6. Clauw DJ, Chrousos
GP. Chronic pain and fatigue syndromes: overlapping clinical and
neuroendocrine features and potential pathogenic mechanisms.
Neuroimmunomodulation. 1997;4:134-153.
7. Russell IJ. The
promise of substance P inhibitors in fibromyalgia. Rheum Dis Clin North Am
. 2002;28:329-342.
8. Engel GL. The need
for a new medical model: a challenge for biomedicine. Science.
1977;196:129-136.
9. Konecna L, Yan MS,
Miller LE, et al. Modulation of IL-6 production during the menstrual cycle in
vivo and in vitro. Brain Behav Immuno. 2000;14:49-61.
10. Middleton GD,
McFarlin JE, Lipsky PE. The prevalence and clinical impact of fibromyalgia in
systemic lupus erythematosus. Arthritis Rheum. 1994;37:1181-1188.
11. Wolfe F, Ross K,
Anderson J, et al. The prevalence and characteristics of fibromyalgia in the
general population. Arthritis Rheum. 1995;38:19-28.
12. Wolfe F. When to
diagnose fibromyalgia. Rheum Dis Clin North Am. 1994;20:485-501.
13. Hudson JI,
Goldenberg DL, Pope HG, et al. Comorbidity of fibromyalgia with medical and
psychiatric disorders. Am J Med. 1992;92:363-367.
14. Giesecke T,
Williams DA, Harris RE, et al. Subgrouping of fibromyalgia patients on the
basis of pressure-pain thresholds and psychological factors. Arthritis Rheum
. 2003;48:2916-2922.
15. Wolfe F, Simons DG,
Fricton J, et al. The fibromyalgia and myofascial pain syndromes: A
preliminary study of tender points and trigger points in persons with
fibromyalgia, myofascial pain syndrome and no disease. J Rheumatol.
1992;19:944-951.
16. Goldenberg DL,
Burckhardt C, Crofford L. Management of fibromyalgia syndrome. JAMA
. 2004;292:2388-2395.
17. Arnold LM, Hess EV,
Hudson JI, et al. A randomized, placebo-controlled, double-blind,
flexible-dose study fluoxetine in the treatment of women with fibromyalgia.
Am J Med. 2002;112:191-197.
18. O'Malley PG, Balden
E, Tomkins G, et al. Treatment of fibromyalgia with antidepressants: a
meta-analysis. J Gen Intern Med. 2000;15:659-666.
19. Bennett RM, Kamin
M, Karim R, Rosenthal N. Tramadol and acetaminophen combination tablets in the
treatment of fibromyalgia pain: a double-blind, randomized, placebo-controlled
study. Am J Med. 2003;114:537-545.
20. Vaeroy H,
Abrahamsen A, Forre O, Kass E. Treatment of fibromyalgia: a parallel double
blind trial with carisoprodol, paracetamol, and caffeine versus placebo.
Clin Rheumatol. 1989;8:245-250.
21. Goldenberg DL,
Mayskiy M, Mossey CJ, et al. A randomized, double-blind crossover trial of
fluoxetine and amitriptyline in the treatment of fibromyalgia. Arthritis
Rheum. 1996;39:1852-1859.
22. Crofford LJ,
Rowbotham MC, Mease PJ, et al. Pregabalin for the treatment of fibromyalgia
syndrome: results of a randomized, double-blind, placebo-controlled trial.
Arthritis Rheum. 2005;52:1264-1273.
23. Arnold LM, Lu Y,
Crofford LJ, et al. A double-blind, multicenter trial comparing duloxetine
with placebo in the treatment of fibromyalgia patients with or without major
depressive disorder. Arthritis Rheum. 2004;50:2974-2984.
24. Tofferi JK, Jackson
JL, O'Malley PG. Treatment of fibromyalgia with cyclobenzaprine: a
meta-analysis. Arthritis Rheum. 2004;51:9-13.
25. Busch A, Schachter
CL, Peloso PM, Bombardier C. Exercise for treating fibromyalgia syndrome.
Cochrane Database Syst Rev. 2002;CD003786.
26. Jones KD,
Burckhardt CS, Clark SR, et al. A randomized controlled trial of muscle
strengthening versus flexibility training in fibromyalgia. J Rheumatol.
2002;29:1041-1048.
27. Tavoni A,
Jeracitano G, Cirigliano G. Evaluation of S-adenosylmethionine in secondary
fibromyalgia: a double-blind study. Clin Exp Rheumatol.1998;16:106-107.
28. Volkmann H,
Norregaard J, Jacobsen S, et al. Double-blind, placebo-controlled crossover
study of intravenous S-adenosyl-L-methionine in patients with fibromyalgia.
Scand J Rheumatol. 1997;26:206-211.
29. Puttini PS, Caruso
I. Primary fibromyalgia syndrome and 5-hydroxy-L-tryptophan: a 90-day open
study. J Int Med Res. 1992;20:182-189.
30. Haanen HCM,
Hoenderdos HTW, Van Romunde LKJ, et al. Controlled trial of hypnotherapy in
the treatment of refractory fibromyalgia. J Rheumatol. 1991;18:72-75.
31. Goldenberg DL,
Kaplan KH, Nadeau MG, et al. A controlled study of a stress-reduction,
cognitive-behavioral treatment program in fibromyalgia. J Musculoskel Pain
. 1994;2:53-66.
To comment on this article,
contact
editor@uspharmacist.com.






