US Pharm. 2007;32(5):HS-20-HS-31.
Central
pain is defined as pain associated with lesions of the central nervous system
that lead to damage of somatosensory pathways.1 It is considered to
be one of the most distressing forms of chronic pain and can be intractable in
many patients. Central pain can be nociceptive and/or neuropathic in nature
and can be precipitated by trauma, stroke, multiple sclerosis, or compression
of cranial nerves. Patient history is the most effective means for diagnosing
central pain, and each syndrome is associated with its own array of cardinal
symptoms. Central pain syndromes are difficult to manage, and complete pain
relief is often unattainable. Reducing pain to a level that is acceptable for
the patient should be the primary goal of therapy. This article will
focus on pharmacologic therapies that have been evaluated in spinal
cord–related pain, brain-related pain, multiple sclerosis–related pain, and
trigeminal neuralgia.
Spinal Cord–Related Pain
Trauma is the most
common cause of spinal cord–related pain, with an incidence rate ranging from
6.4% to 94% according to published estimates.1 Pain after spinal
cord injury can occur immediately or can be delayed for up to five years. When
the onset of pain is delayed beyond one year, more than half of such patients
may suffer from a pathologic lesion in the spinal cord that expands and
damages the center of the cord, a condition known as syringomyelia.2
Although the quality of pain described can vary between patients, there are
three common components: spontaneous steady, spontaneous neuralgic, and evoked
pain. Spontaneous steady pain may occur as a result of deafferentation of
sensory nerves in the central nervous system, resulting in pain that is
expected yet unpredictable. Spontaneous neuralgic pain may be derived from
neural damage and is most commonly described as a burning sensation. Evoked
pain consists of allodynia and/or hyperpathia, conditions where nonnoxious
stimuli such as light touch provoke pain. In any case, classifying pain
related to spinal cord injury can be challenging due to poor localization and
drastic temporal variations. In 2000, an International Association for the
Study of Pain (IASP) task force developed a classification system for patients
with spinal cord–related pain that identifies the pain type, system involved,
and structures or pathology.2
Brain-Related Pain
The majority of
cases of brain-related central pain are caused by strokes. Brain-related
central pain is rare and occurs in only 1% to 2% of all stroke patients, with
90% arising from vascular etiology.1 Central poststroke pain (CPSP)
has been referred to as "thalamic pain," but this term has fallen out of favor
in light of evidence showing that pain can arise from numerous sites within
the brain. Furthermore, it has been suggested that CPSP can arise from a
chemical imbalance between glutamate and gamma-aminobutyric acid (GABA). By
correcting this imbalance, pain relief is possible.1,2 Onset of
CPSP can occur within one to two months after a cerebrovascular accident, but
may be delayed for as long as one to six years after injury. The predominant
characteristics are steady and evoked pain, although neuralgic pain is still
present. Similar to spinal cord–related pain, there is vast interpatient
variability in CPSP. Common symp toms include: muscle
pain, dysesthesias, hyperpathia, allodynia, intermittent shooting/lancinating
pain, circulatory pain, and peristaltic/visceral pain.2
Management of Spinal
Cord–Related and Brain-Related Pain
Nonopioid (i.e.,
NSAIDs) and opioid analgesics are virtually ineffective for the management of
spinal cord–related or brain-related central pain. Other therapeutic classes
that have been investigated include anticonvulsants, antidepressants, N
-methyl-d-aspartate (NMDA) receptor antagonists, and GABA agonists. Based on
evidence from small, double-blind, placebo-controlled trials, intravenous
lidocaine, ketamine, or propofol may be beneficial for short-term pain control
(up to 45 minutes, 30 minutes, and 3 hours, respectively).3-5
Unfortunately, the chronicity of central pain warrants the use of agents that
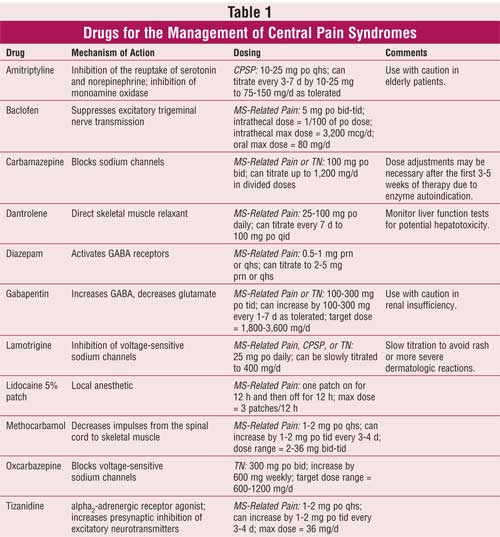
provide long-term relief. Amitriptyline or lamotrigine can be considered as
first-line therapy (TABLE 1).6 Amitriptyline use was
associated with a reduction in pain and improvement in patient global rating
when used in doses of 75 mg po daily over four weeks in a small, double-blind,
placebo-controlled trial of 15 patients with CPSP.7 Vestergaard et
al8 identified that the titration of lamotrigine up to 200 mg po
daily over eight weeks was associated with a reduction in pain scores when
compared to placebo in a small group of patients with CPSP. When evaluated in
patients with spinal cord–related pain, lamotrigine use resulted in a
reduction in brush-evoked allodynia (pain evoked by an innocuous brush) and
wind-up-like pain (pain caused by repeated prickling of the skin).9
Second-line therapies include mexiletine, fluvoxamine and gabapentin; the data
supporting the use of these agents, however, are based on poor-quality studies
and/or anecdotal experience.3,10
Multiple Sclerosis–Related
Pain
Patients suffering
from multiple sclerosis (MS) endure a multitude of symptoms, including pain as
a common complaint. Studies from the past 20 years have indicated a pain
prevalence of 29% to 79% accompanying those afflicted with MS.11
Pain related to MS exists through two possible mechanisms, central
(neuropathic) and musculoskeletal, and may present acutely and/or chronically.
12 Neuropathic pain stems from direct neurologic damage caused by
demyelinating lesions, while musculoskeletal pain generally arises from
reduced mobility.13 Osterberg et al14 identified that
central pain occurs in approximately 28% of patients and that it typically
presents in the early stages of the disease; in some cases, it is the initial
clinical manifestation. Pain will likely increase as the patient's age and the
duration of the disease increase, and may be the only indication of relapse.
Central pain related to MS will predominantly affect the lower extremities,
mainly the legs and feet, but can affect other areas as well.14
Patients with MS who suffer from central pain can have exacerbations
precipitated by light touch, changes in temperature (specifically cold),
physical activity, and emotional stress.15 In 2003, Svendsen et al
found that patients with MS, when compared to reference subjects, described
pain presenting most often as tiring/exhausting (48.6%), shooting (36.3%),
hot/burning (22.9%), cramping (20%), heavy (24.7%), and aching (19.9%).16
Patients receiving interferon therapy to help slow the progression of MS may
also experience muscle aches and headaches.17 In 2004, the National
Collaborating Centre for Chronic Disease, based in London, released guidelines
outlining treatment strategies for the management of MS.13
The initial treatment of
central neuropathic pain related to MS should be with anticonvulsants,
typically carbamazepine (Tegretol) or gabapentin (Neurontin). Tricyclic
antidepressants (TCAs), initiated at low dosages, are useful for dysesthetic
extremity pain. Lidocaine 5% transdermal patches (administered 12 hours on, 12
hours off) can also be considered as first-line therapy. Combinations of more
than one initial treatment may be instituted to provide additional benefit.
NSAIDs are the drugs of choice for patients suffering from musculoskeletal
pain, and methocarbamol (Robaxin), a muscle relaxant, may also be considered.
17,18 Second-line treatments, such as lamotrigine (Lamictal), are
beneficial if a patient is not responding to titrated dosages of carbamazepine
or gabapentin. Lamotrigine should be titrated slowly due to the risk serious
adverse effects. If patients are not responding to TCAs, other antidepressants
such as bupropion (Wellbutrin), citalopram (Celexa), and venlafaxine (Effexor)
may be initiated. Opioid therapy is likely to be effective in patients
suffering from neuropathic pain that is refractory to first-line therapies.
Patients should be initiated on short-acting opioids and titrated up based on
symptom severity. Long-acting opioids should be reserved for chronic
refractory conditions and patients who cannot be adequately controlled on
short-acting medications.17
Other possible treatments for
pain related to MS include capsaicin (Zostrix), which can decrease burning and
tingling of the extremities by interfering with pain transmission;
methylprednisolone for optic neuritis; clonidine; dextromethorphan;
mexiletine; and ketamine.17-19 The use of cannabis has been
investigated in patients with MS. Chong et al demonstrated that almost one
third of surveyed patients were using cannabis illegally in an attempt to
alleviate symptoms. There has been a significant correlation between use and
disability.20 Cannabis has been shown in several studies to help
decrease neuropathic pain as well as spasticity, an increase in muscle tone
that occurs due to demyelination of certain central nervous system pathways,
although controversy surrounding its use remains. Many believe its benefits in
MS are comparable to short-acting opioid therapy, and most governments have
rejected its approval as a viable therapeutic option. The Canada government
recently approved a cannabis extract formulated as an oromusocal spray
(Sativex) for neuropathic pain.21
Spasticity occurs in roughly
75% of patients with MS. Pain can present as exaggerated contractions or as
muscle stiffness. Baclofen (Lioresal), a centrally acting skeletal muscle
relaxant, and tizanidine (Zanaflex), an alpha2-adrenergic receptor
agonist, are the most effective medications prescribed. Baclofen may be
administered as an implantable, intrathecal pump, allowing drug to be
delivered directly to the cerebrospinal fluid. This requires surgery, and both
infection and withdrawal are possible complications. Botulinum toxin (Botox)
injections may be used if a patient is suffering from localized, focal
spasticity. Injections are repeated every three to four months and are very
expensive.17,22 Diazepam (Valium) and dantrolene (Dantrium) should
only be considered in patients nonresponsive to other therapies.
Trigeminal Neuralgia (tic
douloureux)
Trigeminal neuralgia (TN), or tic
douloureux, is defined as sudden, severe, and recurrent unilateral facial
pain. It is considered to be a disease of the elderly, with a peak incidence
between the ages of 50 and 70.23,24 Sixty percent of patients
diagnosed with TN are female, and no racial or ethnic predisposition has been
identified.23 Classic TN, formerly known as idiopathic TN, accounts
for 80% to 90% of cases and may be attributed to compression of the trigeminal
nerve by an anomalous loop of artery or vein that results in nerve
demyelination.24 The superior cerebellar artery is the compressing
vessel in almost 75% of cases.25 Benign tumors, such as
meningiomas, or MS is identified in less than 10% of patients presenting with
symptomatic TN. It is unclear how nerve demyelination or compression lesions
cause the symptoms characteristic of TN. Neuronal hyperactivity, altered
peripheral nerve sensitivity, and increased sensitivity to chemical and
mechanical stimuli may explain the spontaneity of pain onset and cessation.
23-25 Furthermore, neuronal hypersensitivity can mimic focal epilepsy,
thus possibly explaining the role of anticonvulsants in the pharmacologic
management of TN.
TN is characterized by
shock-like stabbing pain that is unilateral and abrupt in onset and
termination, and is precipitated by nonnoxious stimuli. It is rarely
accompanied by sensory loss.26 Pain is brief, lasting only a few
seconds, and paroxysmal, with absence of pain in between episodes. Pain is
provoked by the nonnoxious stimulation of trigger zones that can arise from
cutaneous areas innervated by the trigeminal nerve or from teeth or oral
mucosa.23 Cutaneous triggers include gently touching the face or
shaving and mostly arise from the anterior regions of the face. Brushing the
teeth, chewing, swallowing, or talking can also trigger paroxysms that arise
from the oral region. Brief spasms of the facial muscles may accompany any
episode. Other symptoms such as lacrimation or rhinorrhea rarely occur.25
Considered an intermittent disease, months to years can pass in between
painful episodes of TN. When the patient experiences a recurrence, it is
almost always in the same facial region, which can expand over time.23-25
In patients experiencing facial pain, other more common causes that are
distinguishable from TN should be investigated. These include dental pain,
temporomandibular joint pain, cluster headaches, migraines, and persistent
idiopathic facial pain.24 In the absence of clinically useful
diagnostic studies, patient history and dental examination are used to
establish the presence of TN. Magnetic resonance imaging can visualize a
vascular compression lesion or tumor, but this test is reserved for patients
considering surgical treatment options.24
Anticonvulsants are considered
the mainstay of therapy for TN. Carbamazepine is FDA approved for the
treatment of TN in adults and is considered the drug of choice. Although its
mechanism of action is not fully understood, carbamazepine is thought to
reduce neuronal hypersensitivity by blocking voltage-sensitive sodium channels.
27 A systematic review of four placebo-controlled trials found that
carbamazepine improved pain scores and reduced pain intensity in patients with
TN.28 When compared to active control, carbamazepine was found to
be superior to tizanidine and less effective than pimozide.28 Small
sample sizes, variation in dosing between trials (400–2400 mg/day), and lack
of standardized measures are just a few limitations that demonstrate the need
for high-quality studies in this population. However, the rarity and
spontaneity of TN may preclude this.
The recommended initial dose of
carbamazepine is 100 mg orally twice daily and can be increased by 50 to 100
mg every three to four days, with a maximum recommended daily dose of 1,200
mg. Due to its ability to act as an autoinducer of cytochrome P-450 3A4, a
dose adjustment may be warranted after the first three to five weeks of
therapy, the time at which autoinduction is complete in patients managed on a
fixed-dose regimen.27 The normal therapeutic range for the
treatment of neuralgias is 2 to 7 mcg/mL, and concentrations measured during
the first few weeks of therapy should be evaluated cautiously due to enzyme
autoinduction. Carbamazepine is associated with several adverse effects
including drowsiness, ataxia, photosensitivity, and blurred vision. More
serious adverse effects include bone marrow suppression, hepatitis, and
hyponatremia, and complete blood counts, liver function tests, and serum
sodium levels should be evaluated prior to therapy and periodically
thereafter. Oxcarbazepine may be considered as an alternative to carbamazepine
due to its similar mechanism of action and more favorable adverse effect
profile24; however, efficacy data in this population are derived
from uncontrolled studies, and further evaluation is needed.
In patients who fail or cannot
tolerate carbamazepine therapy, choice of therapy becomes less clear. Several
other agents have been evaluated, but evidence supporting their use is weak
and may be limited due to intolerable adverse effects. Anticonvulsants that
can be considered as second-line therapy include gabapentin, lamotrigine, and
phenytoin.29,30 Baclofen may be useful in patients with TN
associated with MS.31 When pharmacologic interventions have been
exhausted, surgical options should be explored. Available procedures with high
initial response rates include microvascular decompression of the trigeminal
nerve and nerve ablation.24 Microvascular decompression is
associated with long-term pain relief and a low risk of sensory loss.
Discussion
Historically, there has been limited
information regarding treatment options for central pain syndromes. As the
pathophysiology becomes increasingly understood, new therapeutic options have
emerged and the role of existing pharmacotherapeutic agents has expanded. Due
to varying mechanisms of pain, medication selection and dosage are both
issues. Certain medications will, in fact, have differing dosages based on the
syndrome being treated. Pharmacists can play an integral role in drug
selection based on the type of central pain that is being treated. In
addition, therapeutic monitoring for several pharmacologic agents is essential
for adequate and sustained patient care. This includes pain assessment,
compliance issues, adverse drug reactions, and, in some instances, monitoring
therapeutic levels. Through close patient interaction and attention to
specific symptoms, pharmacists can make sound interventions to help patients
avoid potential complications and achieve appropriate analgesia.
References
1. Loeser JD, ed. Bonica's Management of Pain. 3rd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2001:434-457.
2. Nicholson BD. Evaluation and treatment of pain syndromes. Neurology. 2004;62(suppl 2):S30-S36.
3. Attal N. Chronic neuropathic pain: mechanisms and treatment. Clin J Pain.2000;16(suppl 3):S118-S130.
4. Canavero S, Boncalzi V, Pagni CA, et al. Propofol analgesia in central pain: preliminary clinical observations.
J Neurol. 1995;242:561-567.
5. Backonja M, Arndt G, Gombar K, et al. Response of chronic neuropathic pain syndromes to ketamine: a preliminary study. Pain. 1994;56:51-57.
6. Frese A, Husstedt IW, Ringelstein EB, et al. Pharmacologic treatment of central post-stroke pain. Clin J Pain . 2006;22:252-260.
7. Leijon G, Boivie J. Central post-stroke pain: a controlled trial of amitriptyline and carbamazepine. Pain.1989;36:27-36.
8. Vestergaard K, Andersen G, Gottrup H et al. Lamotri gine for central post-stroke pain: a randomized, controlled trial. Neurology.2001;56:184-190.
9. Finnerup NB, Sindrup SH, Bach FW. et al. Lamotri gine in spinal cord injury pain: a randomized controlled trial. Pain. 2002;96:375-383.
10. Hansson P. Post-stroke pain case study: clinical characteristics, therapeutic options and long-term follow-up. Eur J Neurol. 2004;11(suppl 1):22-30.
11. Clifford DB, Trotter JL. Pain in multiple sclerosis. Arch Neurol. 1984;41:1270-1272.
12. Ehde DM, Osborne TL, Hanley MA, et al. The scope and nature of pain in persons with multiple sclerosis. Multiple Sclerosis. 2006;12:629-638.
13. National Collaborating Centre for Chronic Conditions. Multiple sclerosis. National clinical guideline. London, England: National Institute for Clinical Excellence (NICE); 2004.
14. Osterberg A, Boivie J, Thuomas KA. Central pain in multiple sclerosis–prevalence and clinical characteristics. Eur J Pain. 2005;9:531-542.
15. Wall PD, Melzack R, eds. Textbook of Pain. 4th ed. New York, NY: Churchill Livingstone; 1999:879-914.
16. Svendsen KB, Jensen TS, Overvad K, et al. Pain in patients with multiple sclerosis: a population-based study. Arch Neurol. 2003;60:1089-1094.
17. Maloni HW. Pain in multiple sclerosis: an overview of its nature and management. J Neurosci Nurs. 2000;32:
139-144.
18. Dworkin RH, Backonja M, Rowbotham MC, et al. Advances in neuropathic pain: diagnosis, mechanisms, and treatment recommendations. Arch Neurol. 2003;60:
1224-1234.
19. Sakai T, Tomiyasu S, Ono T, et al. Multiple sclerosis with severe pain and allodynia alleviated by oral ketamine. Clin J Pain. 2004;20:375-376.
20. Chong MS, Wolff K, Wise K, et al. Cannabis use in patients with multiple sclerosis. Multiple Sclerosis . 2006;12:646-651.
21. Barnes MP. Sativex: clinical efficacy and tolerability in the treatment of symptoms of multiple sclerosis and neuropathic pain. Expert Opin Pharmacother. 2006;7:607-615.
22. Schwendimann RN. Treatment of symptoms of multiple sclerosis. Neurol Res. 2006;28:306-315.
23. Loeser JD, ed. Bonica's Management of Pain. 3rd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2001:855-860.
24. Bennetto L, Patel NK, Fuller G. Trigeminal neuralgia and its management. BMJ. 2007;334:201-205.
25. Truini A, Galeotti F, Cruccu G. New insight into trigeminal neuralgia. J Headache Pain. 2005;6:237-239.
26. Nurmikko TJ. Altered cutaneous sensation in trigeminal neuralgia. Arch Neurol. 1991;48:523-527.
27. Tegretol [package insert]. East Hanover, NJ, Novartis Pharmaceuticals Corp.; September 2006.
28. Wiffen PJ, McQuay HJ, Moore RA. Carbamazepine for acute and chronic pain. Cochrane Database of
Systematic Reviews 2006;4.
29. Wiffen PJ, McQuay HJ, Edwards JE, et al. Gabapentin for acute and chronic pain. Cochrane Database of Systematic Reviews 2006;4.
30. Wiffen PJ, Collins S, McQuay H, et al. Anticonvulsant drugs for acute and chronic pain. Cochrane Database of Systematic Reviews 2006;4.
31. He L, Wu B, Zhou M.
Non-antiepileptic drugs for trigeminal neuralgia. Cochrane Database of
Systematic Reviews 2006;4.
To comment on this article, contact
editor@uspharmacist.com.





