US Pharm. 2007;33(1):32-37.
Individuals with chronic pain that
lasts for more than three to six months may experience multiple types of pain
in the head and neck region, including headache and facial pain.1
Approximately 18% of women and 6% of men suffer from some form of frequent
headaches, and many cases go undiagnosed and undertreated.2
Headaches have a major socioeconomic impact on society.
This article will review the classifications and pathogenesis of migraine,
various pharmacologic and nonpharmacologic treatments, and the pharmacist's
role in patient education.
Classification
The International
Headache Society has developed a classification system for headache disorders (
TABLE 1).3 Headaches are broadly classified into primary and
secondary headaches. Primary headache disorders, which are due to a primary
neurologic process without an underlying cause, include migraine, tension-type
headache, cluster headache, and other trigeminal autonomic cephalalgias.
Primary headache disorders are subdivided one, two, or three times into
headache types, subtypes, and subforms based on the presence or absence of
symptoms or on the frequency of attacks.3,4
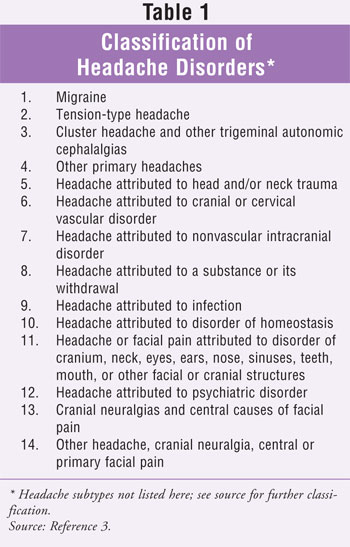
Secondary headache disorders
have a specific underlying cause. These headaches can be attributed to such
causes as head and/or neck trauma; infection; a substance or its withdrawal;
cranial or cervical vascular disorders; nonvascular intracranial disorders;
psychiatric disorders; and disorders of the cranium, neck, eyes, ears, nose,
sinuses, teeth, mouth, or other facial or cranial structures.
Epidemiology
In the United
States, migraine affects approximately 28 million people.5 The
prevalence of migraine is similar for boys and girls in the prepubescent
years, but is higher in adolescent girls than boys. In adulthood, migraine is
three times more frequent in women than in men; about 75% of all individuals
who experience migraines are women.6
Diagnosis
The word migraine
comes from the Greek word hemicrania, meaning "pain on one side of the
head." The World Health Organization ranks migraine 19th of all diseases
worldwide causing disability.7 Migraine, predominately an inherited
disorder, is divided into two major subtypes: migraine without aura and
migraine with aura. Although it is considered a type of primary headache,
migraine can be a secondary headache if it occurs for the first time in close
temporal relation to another disorder that is a known cause of headache.
Migraine attacks are commonly unilateral and throbbing, and the pain is
aggravated by routine activities such as walking, climbing stairs, or bending
over.
Diagnosis of migraine is
difficult because of the periodic nature of the condition and the absence of
radiographic and laboratory markers of disease. Reliance on the patient's
ability to describe past attacks is important for diagnosis.
Phases and Pathogenesis
Migraine is a
neurochemical reaction involving the trigeminovascular system rather than a
vascular event, as was once believed. Although vascular changes do occur, they
are not related to the clinical features of the migraine.8
Stimulation of the trigeminal nerve causes the release of vasoactive peptides;
this is responsible for the head pain, as well as the facial and neck pain,
experienced during migraine. The facial and neck pain often lead to
misdiagnosis of the migraine as a sinus or tension headache.8
A migraine has four phases:
prodrome, aura, headache (pain), and postdrome.9 Not all
migraineurs experience all four phases.
Prodrome:
The prodrome, which occurs hours or days before (or sometimes during) the
headache, is characterized by altered mood, irritability, depression or
euphoria, stiff neck, light sensitivity, yawning, excessive sleepiness,
tiredness, fluid retention, and food cravings. These symptoms occur in 40% to
60% of migraineurs.10
The exact etiology of prodrome
is not fully understood, but it is hypothesized that prodrome is caused by a
dysfunction in the hypothalamus.11
Migraine with Aura:
Migraine with aura is characterized by episodes of neurologic symptoms
including visual, sensory, or motor dysfunction, or a combination of these.
Most aura symptoms, which usually precede (hours or days before) or sometimes
occur with the migraine, develop gradually over five to 20 minutes and last
less than 60 minutes. Aura represents a transient episode of focal neurologic
dysfunction caused by an imbalance between excitatory and inhibitory neuronal
activity at different levels in the central nervous system.11
Visual aura, which is present in up to 99% of migraineurs, may manifest as
bright flashing lights, specks of light, geometric shapes, shimmering, or
scotoma (partial obliteration or loss of vision in a portion or the whole of
the visual field).12 It has been postulated that some of the
surreal adventures depicted in Alice in Wonderland were based on visual
auras experienced by the author, Lewis Carroll.13 It is believed
that visual aura is caused by a wave of cortical spreading depression (CSD)
moving across the cerebral cortex and resulting in depressed neuronal activity
and then intense neuronal activity. In migraineurs who experience visual aura,
CSD may occur in areas of the brain that are "clinically silent" in those who
do not experience visual aura.8,14,15
Sensory aura, which occurs in up to 40% of migraineurs, may take the form of a
paresthesia that involves the arms, face, hands, or other parts of the body.
It also may present as cheiroaural numbness, which is a tingling followed by
numbness starting in the hand, moving superiorly up the arm, and then jumping
to the face, where it is felt around the mouth.16
Migraine Without Aura:
To establish a diagnosis of chronic migraine without aura, five attacks
lasting for four to 72 hours must have occurred on 15 or more days a month for
more than six months. Migraine without aura is usually associated with
photophobia (sensitivity or intolerance to light), phonophobia (fear of
sounds, including one's own voice), nausea, and vomiting; some patients
experience cutaneous allodynia (pain evoked by normally nonpainful stimulus of
the skin) during an attack.11
Individuals who experience migraine with aura also may experience attacks of
migraine without aura. Conversely, however, those who experience migraine
without aura will not experience migraine with aura.11
Headache/Pain:
Headache begins during or within 60 minutes of the aura and is usually
unilateral and throbbing. Although vascular changes are evident during a
migraine, the cause of the headache is neurologic, not vascular. Migraine
headache pain is induced primarily by vasodilation and inflammation leading to
nociception (perception of pain) and central and peripheral sensitization.
Stimulation of the trigeminal nerve (fifth cranial nerve), which carries
sensory information from the face, can cause referral of pain to any of the
nerve's three branches, resulting in facial pain. It can also cause referred
pain to the sensory nerves of the posterior head and neck, resulting in neck
pain.8,11,17
Perivascular nerve activity also results in the release of substances such as
substance P, neurokinin A, calcitonin gene-related peptide, and nitric oxide,
which interact with the blood-vessel wall to produce dilation, protein
extravasation, and sterile inflammation, stimulating the trigeminocervical
complex.9 Substance P, a short-chain polypeptide, is a chemical
messenger that, when released, signals the brain to feel pain.18
Additionally, activation of vascular 5-HT2B and/or 5-HT7
(serotonin receptors), possibly as a consequence of the sudden rise in 5-HT
levels at the onset of a migraine, hypothetically would result in the dilation
of cerebral blood vessels and the concomitant activation of sensory
trigeminovascular nerves, initiating the manifestation of head pain. At this
stage in the migraine process, the activation of specific subtypes of 5-HT
1 receptors has proven clinically effective for relieving migraine pain.
The recent availability of subtype-selective 5-HT1D and 5-HT1F
receptor agonists could possibly lead to antimigraine drugs with a safer
cardiovascular profile.19
Postdrome: About 25%
of migraineurs experience a postdrome, which involves changes in mood and
behavior after the migraine attack. Precipitating factors include caffeine
(and caffeine withdrawal), menstruation, stress, smoking, lack of sleep,
certain foods, and strenuous exercise.11
Migraine Triggers
Various factors can
trigger migraines, including stress, emotions (e.g., depression, anxiety),
hormonal changes (e.g., menstruation, pregnancy, birth control pills), weather
changes, fumes and vapors (e.g., smoke, perfume), lack of sleep, bright light,
noises, and foods. Some foods and additives that can trigger migraines are
monosodium glutamate (also known as MSG), alcohol, tyramine-containing foods
(e.g., pickled herring, aged cheese, cured meats, yeast), chocolate, excessive
caffeine, and nitrites. Migraine triggers are different for each person.
Drug Therapy
Only one-half of
patients seek medical attention for migraine, and only about half of these are
properly diagnosed.20 Drug therapy aims to abort a migraine at the
time it occurs, provide symptomatic pain relief, and prevent a migraine from
recurring.21 Any symptomatic drug therapy, whether prescription or
OTC, should not be used more than twice a week; beyond that, the patient
should be taking preventive medications. The patient should start by
eliminating all products containing caffeine, which causes vasoconstriction.
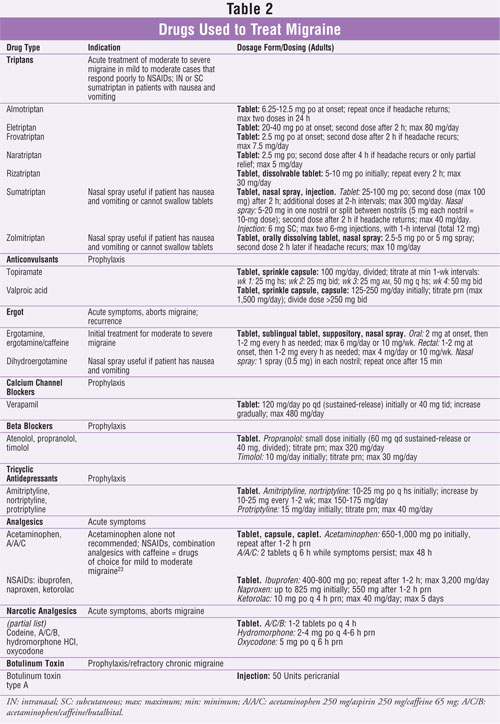
The following are classifications of drugs used in the treatment of acute
migraine attacks and for prophylaxis (TABLE 2).
Abortive Treatment of Acute
Migraine
Triptans:
Introduced in the United
States in the late 1990s, triptans (hydroxytryptamine receptor agonists) are
effective and well tolerated for the initial treatment of acute moderate or
severe migraine to abort the attack or in patients with mild to moderate
migraine who respond poorly to NSAIDs.22,23 A recent study found
sumatriptanñnaproxen to be more effective than monotherapy.24
Triptans bind with high affinity to 5-HT1B/1D receptors and are
referred to as selective serotonin agonists. Activation of these receptors
results in cranial-vessel constriction, inhibition of neuropeptide release,
and reduction of transmission in trigeminal pain pathways. Formulations
available include oral, suppository, injection, and nasal spray. Orally
administered triptans provide pain relief within 30 minutes, and injected
sumatriptan has an onset of action of less than 15 minutes.
Triptans are metabolized primarily by monoamine oxidase enzymes, similar to
monoamine oxidase (MAO) inhibitors. Thus, taking triptans and MAO-A inhibitors
together generally leads to an increase of blood triptan levels. It is
necessary to wait more than two weeks after the MAO inhibitor is discontinued
before initiating triptan therapy.
Triptans should not be administered to patients with ischemic heart disease
(e.g., angina pectoris, history of myocardial infarction, silent ischemia),
symptoms of ischemic heart disease, or coronary-artery vasospasm. Triptans may
increase blood pressure and should not be given to patients with uncontrolled
hypertension. Velentgas et al, however, found no association between triptans
and increased risk of any ischemic events.25
The combined use of triptans and antidepressants, including selective
serotonin reuptake inhibitors (SSRIs) and selective serotonin/norepinephrine
reuptake inhibitors (SNRIs), may cause serotonin syndrome resulting from
excessive blood levels of serotonin; however, the risk is low.26,27
Signs and symptoms include restlessness, hallucinations, rapid heartbeat,
diarrhea, nausea, vomiting, and rapid changes in blood pressure. Serotonin
syndrome is more likely to occur when starting or increasing the dose of a
triptan, SSRI, or SNRI. This combination is not contraindicated, but care
should be taken when the two drugs are given concurrently.
Common adverse reactions with triptans are head and jaw discomfort, flushing,
dizziness, sleepiness, and tiredness.
Ergot Derivatives:
Drugs such as ergotamine and dihydroergotamine nasal spray are
alpha-adrenergic blockers and vasoconstrictors of cranial smooth muscle and
are used in the treatment of moderate or severe migraine in selected patients.
23 Caffeine, a vasoconstrictor, is added to enhance absorption and
potentiate analgesia.28 Elevated blood levels of ergot derivative
occur when the drug is taken with erythromycin and clarithromycin. Many
adverse effects, including nausea, localized edema and itching, and numbness
and tingling in the fingers and toes preclude ergot derivatives for long-term
use or for prevention. Prolonged use may cause medication-overuse headache
(MOH; formerly known as rebound headache). Er!= gotamine derivatives are
contraindicated during pregnancy or in patients with peripheral vascular
disease, hepatic or renal disease, coronary artery disease, hypertension, or
sepsis.
Analgesics:
For mild migraine attacks, analgesics alone or in combination with caffeine
are the drug of choice.29 Overuse of analgesics and caffeine can
aggravate the migraine (i.e., cause MOH). Most of the pain-relievers patients
use are OTC. Caffeine is added to enhance the drug's absorption and to
potentiate the drug's activity. Excedrin Migraine (which is identical to
Excedrin Extra Strength) contains acetaminophen, aspirin, and caffeine. Two
tablets contain roughly the amount of caffeine found in a cup of coffee.
Long-term use of analgesics is discouraged, as this may lead to MOH upon
withdrawal. Adverse effects include nausea and gastrointestinal upset and
bleeding. NSAIDs (e.g., ibuprofen, naproxen) reduce the release of serotonin
and can be used in combination with triptans.21
Narcotic analgesics, which are used for more severe pain, are not
FDA-approved. They may carry a greater risk of MOH, and they have the
potential for abuse and dependency. Refractory patients may require narcotic
injections for acute attacks.30
Migraine Prophylaxis
Choosing a drug for prevention is
based upon the adverse-effect profile of the drug and on the patient's medical
status. Prophylaxis should reduce or eliminate the need for abortive drugs.
Anticonvulsants:
Topiramate is approved for migraine prevention in adults.31 It is a
sulfamate-substituted monosaccharide with a broad spectrum of anticonvulsant
activity. Common adverse effects include lowered bicarbonate levels in the
blood causing an increase in blood acidity (metabolic acidosis),
hyperventilation, and fatigue. Adequate fluid intake is important to minimize
the risk of renal-stone formation. Other side effects are tingling in the arms
and legs, loss of appetite, nausea, diarrhea, taste change, and weight loss.
32
Valproic acid is approved for migraine prophylaxis and can take up to two to
three weeks to be effective. Common adverse effects, including weight gain,
sedation, and xerostomia, may preclude its use in some patients.
Beta Blockers: The
use of beta blockers for the treatment of migraine started in the 1960s, when
patients being treated for heart problems found that their migraine frequency
decreased. The reason for the drugs' effectiveness may be that they limit the
tendency for cranial blood vessels to overdilate. It may take up to four to
six weeks to see a reduction in migraine frequency. Timolol and propranolol
are FDA-approved for prophylaxis, but propranolol has more research evidence
of efficacy than timolol.
Calcium Channel Blockers:
Similar to beta blockers, calcium channel blockers were originally used to
treat cardiovascular conditions. These drugs also may work by stabilizing
blood-vessel membranes by preventing them from overdilating. It can take up to
two months to see effects.
Tricyclic Antidepressants:
Antidepressants are used
for migraine prevention for their analgesic effect. A lower dose is prescribed
than would be used for the treatment of depression. It can take up to three to
four weeks before the drug is effective.33
Botulinum Toxin Type A:
In addition to being
used cosmetically and for dystonia (sustained contraction of muscles),
botulinum toxin type A--which is derived from the exotoxin produced by the
bacterium Clostridium botulinum--is used for the prevention of
migraines for up to six months and for refractory chronic migraine in patients
who previously failed to respond to at least three prophylactic medications.
Although the exact mechanism is unclear, it has been hypothesized that the
drug works by inhibiting the release of transmitters from pain-sensitive nerve
endings.34
Alternative Treatments:
Some alternative remedies used in the prophylaxis of migraine are feverfew,
riboflavin, coenzyme Q10, magnesium, butterbur, and melatonin. There are no
randomized, controlled studies of melatonin.35,36 There is concern
about the lack of standardization of the contents and the purity of herbal
supplements.
A number of alternative
modalities have been recommended for the treatment and prevention of migraine,
including hypnosis, biofeedback, meditation, acupuncture, massage, and
transcutaneous electrical nerve stimulation.
MOH
MOH is a syndrome
or cycle that occurs when a patient overuses medications of different classes
(but not of a single class), which contributes to the headache rather than
easing it.37 MOHs can occur in headache-prone individuals when
acute headache medications are taken for other indications. OTC pain relievers
containing caffeine (e.g., Excedrin Migraine, Excedrin Tension Headache) are a
possible cause; caffeine in coffee, sodas, and various other foods and
beverages also may contribute to MOH. To prevent MOH, the amount of pain
medication being used should be reduced (limited to two days per week) or
stopped. MOH is difficult to diagnose. The signs and symptoms of MOH include
nausea, anxiety, insomnia, and restlessness.
Conclusion
Migraine places a
significant burden not only on patients, but on their families and employers
as well. Many types of headache are associated with temporary disability
(e.g., missed work, school, and household responsibilities) and with high
personal and socioeconomic costs. Since many people suffer from migraines, the
pharmacist plays a pivotal role in patient education.
Pharmacists should take a
proactive approach in managing patients with migraines and other types of
headache. To do this more effectively, the pharmacist must have a good
understanding of the physiologic and neurologic processes involved in headache
disorders and a broad knowledge of the available pharmacologic treatments.
References
1. Mehta SA,
Epstein JB, Greene C. Recognition and management of headache. J Can Dent
Assoc. 2006;72:835-839.
2. Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine in the
United States. JAMA. 1992;267:64-69.
3. Headache Classification Subcommittee of the International Headache Society.
The International Classification of Headache Disorders. 2nd ed.
Cephalalgia. 2004;24(suppl 1):1-150.
4. Olesen J, Bousser MG, Diener HC, et al. New appendix criteria open for a
broader concept of chronic migraine. Cephalalgia. 2006;26:742-!=746.
5. Lipton RB, Diamond S, Reed M, et al. American Migraine Study II:
prevalence, burden, and health care utilization for migraine in the United
States. Headache. 2000;40:416.
6. Stewart WF, Linet MS, Celentano DD, Van Natta M, Ziegler D. Age- and
sex-specific incidence rates of migraine with and without visual aura. Am J
Epidemiol. 1991;134:1111-1120.
7. World Health Organization. Headache Disorders and Public Health.
Education and Management Implications. Geneva; 2000.
8. Welch KM. Contemporary concepts of migraine pathogenesis. Neurology.
2003;61(suppl 4):S2-S8.
9. Goadsby PJ, Lipton RB, Ferrari MD. Migraine--current understanding and
treatment. N Engl J Med. 2002;346:257-270.
10. Silberstein SD, Lipton RB, Goadsby PJ, eds. Headache in Clinical
Practice. 2nd ed. London, England: Martin Dunitz Ltd; 2002.
11. Monographs in Medicine. A Study of Migraine. 12th ed. Rahway, NJ:
Merck & Co, Inc; 2005.
12. Podoll K, Robinson D. Illusory splitting as visual aura symptom in
migraine. Cephalalgia. 2000;20:228-232.
13. Podoll K, Robinson D. Lewis Carroll's migraine experiences. Lancet
. 1999;252:1366.
14. Silberstein SD. New developments in headache and migraine. Paper presented
at: 57th Annual Meeting of the American Academy of Neurology; April 9-16,
2005; Miami Beach.
15. Lauritzen M. Pathophysiology of the migraine aura. The spreading
depression theory. Brain. 1994;117:199-210.
16. Cutrer FM, Black DF. Imaging findings of migraine. Headache.
2006;46:1095-1107.
17. Hargreaves RJ, Shepheard SL. Pathophysiology of migraine--new insights.
Can J Neurol Sci. 1999;26(suppl 3):S12-S19.
18. DeVane CL. Substance P: a new era, a new role. Pharmacotherapy.
2001;21:1061-1069.
19. Hamel E. The biology of serotonin receptors: focus on migraine
pathophysiology and treatment. Can J Neurol Sci.1999;26:S2-S6.
20. Lipton RB, Stewart WR, Celentano DD, Reed ML. Undiagnosed migraine
headaches. A comparison of symptom-based and reported physician diagnosis.
Arch Intern Med. 1992;152:1273-1278.
21. Schuurmans A, van Weel C. Pharmacologic treatment of migraine: comparison
of guidelines. Can Fam Physician. 2005;51:838-843.
22. Lipton RB, Bigal ME, Goadsby PJ. Double-blind clinical trials of oral
triptans vs other classes of acute migraine medication ñ a review.
Cephal!=algia. 2004;24:321-332.
23. Silberstein SD. Practice parameter: evidence-based guidelines for migraine
headache (an evidence-based review): report of the Quality Standards
Subcommittee of the American Academy of Neurology. Neurology.
2000;55:754-762.
24. Brandes JL, Kudrow D, Stark SR, et al. Sumatriptan-naproxen for acute
treatment of migraine. A randomized trial. JAMA. 2007;297:1443-1454.
25. Velentgas P, Cole JA, Mo J, et al. Severe vascular events in migraine
patients. Headache. 2004;44:642-651.
26. Wooltorton E. Triptan migraine treatments and antidepressants: risk of
serotonin syndrome. CMAJ. 2006;175:874.
27. Food and Drug Administration/Center for Drug Evaluation and Research.
Information for healthcare professionals: selective serotonin reuptake
inhibitors (SSRIs), selective serotonin-norepinephrine reuptake inhibitors
(SNRIs), 5-hydroxytryptamine receptor agonists (triptans). Available at:
www.fda.gov/CDER/DRUG/InfoSheets/HCP/triptansHCP .htm. Accessed December 20,
2007.
28. Schiff PL. Ergot and its alkaloids. Am J Pharm Educ. 2006;70:98.
29. Wenzel RG, Sarvis CA, Krause ML. Over-the-counter-drugs for acute migraine
attacks: literature review and recommendations. Pharmacotherapy.
2003;23:294-505.
30. Von Seggern RL, Adelman JU. Oral narcotic protocol to reduce narcotic
injections in refractory migraine patients. Headache. 1997;37:!=
341-345.
31. Silberstein SD, Neto W, Schmitt
J, Jacobs D, for the MIGR-001 Study Groups. Topiramate in migraine prevention:
results of a large controlled trial. Arch Neurol. 2004;61:490-495.
32. Krymchantowski A, Tavares C. Weight variations in patients receiving
topiramate migraine prophylaxis in a tertiary care setting. Medscape Gen Med
. 2004;6:48.
33. Lynch ME. Antidepressants as analgesics: a review of randomized controlled
trials. J Psychiatry Neurosci. 2001;26:30-36.
34. Dodick DW, Mauskop A, Elkind AH, et al. Botulinum toxin type A for the
prophylaxis of chronic daily headache: subgroup analysis of patients not
receiving other prophylactic medications: a randomized double-blind,
placebo-controlled study. Headache. 2005;45:315-324.
35. Evans RW, Taylor FR. "Natural" or alternative medications for migraine
prevention. Headache. 2006;46:1012-1018.
36. Lipton RB, G^bel H, Einh‰upl M, et al. Petasites hybridus
root !=(butterbur) is an effective preventive treatment for migraine.
Neurology. 2004;63:2240-2244.
37. Silberstein SD, Olesen J, Bousser M-G, Diener H-C, et al. The
International Classification of Headache Disorders, 2nd Edition
(ICHD-II)--revision of criteria for 8.2 Medication-overuse headache .
Cephalalgia. 2005;25:460-465.
To comment on this article, contact
editor@uspharmacist.com.





