US Pharm . 2007;32(6):HS33-HS37.
Pain is a common and often undertreated phenomenon in patients 65 and older that is often attributed to physical injuries and trauma or may stem from a range of disease states. One study conducted in 1997 found that 18% of older Americans take analgesics several times a week or more and 45% of patients taking chronic medications had visited three or more doctors within the previous five years.1 In addition, an estimated 45% to 80% of nursing home residents experience pain that contributes to a decreased quality of life (QOL) and limited functional ability.2 Persistent pain in older patients is commonly associated with depression, anxiety, impaired ambulation, sleep disturbances, and decreased socialization.3 Increasing awareness of barriers to care, age-related physiologic changes, and concomitant diseases and medications that will impact drug selection is especially important for health professionals caring for the growing elderly population to ensure safe and effective pain management.
Misconceptions About Pain Management in the Elderly Population
Misconceptions and attitudinal barriers held by family members, health care providers, and patients themselves regarding pain management in the elderly contribute to the large number of patients in this population who have pain that is inadequately treated. Perhaps at the root of these misconceptions is that elderly patients experience pain to a lesser degree compared to younger patients. This belief stemmed from the idea that pain transmission has shifted predominantly to C fiber involvement as compared to A delta fibers. Other barriers to care and misconceptions include the perception that pain is a normal part of the aging process; fear of addiction to or dependence on opioid medications; the idea that patients who report pain have "drug-seeking" behaviors; and the view of pain as a symbol of weakness that should be endured. 4-6 Pain that responds poorly to various treatment modalities and/or pain with an unidentified etiology can cause health care provider discouragement and frustration. Fear of repercussions for overprescribing opioids and a lack of training in the area of pain management among health care providers may also contribute to subtherapeutic pain responses.7
Though clinical trials have shown mixed results regarding alterations in pain perception among elderly patients, the American Geriatrics Society (AGS) concludes that these alterations are likely to be clinically insignificant.3,4 Thus, the recognition of barriers and misconceptions about pain management in the elderly is imperative to appropriately educate patients, family members, care givers, and other health care providers in order to provide adequate pain relief.
Challenges of Pain Assessment in the Elderly
With the knowledge that pain is often inadequately treated in the elderly population due to underlying misconceptions, any report of pain that impacts physical or psychosocial functioning or reduces patient QOL should be recognized as a significant problem and managed appropriately.3 In fact, pain is often considered the "fifth vital sign" and should be questioned at every health care visit. Patients who present with pain should undergo a comprehensive pain assessment. Due to the subjective nature of pain, measures such as the Numerical Rating Scale and Verbal Descriptor Scale have been developed and implemented to provide more objective data. Use of the pain thermometers or face scales may be necessary for patients with cognitive impairment who have difficulty responding to numerical pain scales. Pain scales focused on "pain relief" may be more beneficial than those focused on "pain intensity," as patients will have the same baseline of "relief," whereas "intensity" is highly patient dependent.4 Pain descriptors such as location, duration, onset, frequency, exacerbating and alleviating factors, intensity, and quality should be assessed, specifically asking the patient to describe in his or her own words what the pain feels like. This assessment should also include a list of prescription, OTC, and complementary alternative medications that have been attempted by the patient along with the response to treatment and nonpharmacologic interventions such as thermal or ice packs, biofeedback techniques, and acupuncture. In addition, it is important to determine how satisfied the patient is with his or her current pain management. Allowing ample time for patient response to questions and repeating of questions will be necessary in some cases to obtain a complete pain history.3,4
Pain assessment in elderly patients with moderate-to-severe dementia, Parkinson's disease, or stroke or in those who cannot verbally communicate may be problematic. Thus, querying caregivers and/or family members who frequently observe patients with any of these conditions may be beneficial. Behaviors that may indicate pain include gait or mobility changes, moaning and groaning, rapid blinking, calling out for help, appetite or sleep changes, crying, irritability, guarding, facial distortion, frowning or grimacing, increased wandering, aggression, combativeness, fidgeting, and restrictive movements. It is important to note that these behaviors are not specific to patients who have difficulty communicating verbally and are important when assessing any elderly patient. The physical examination of an older adult with reports of pain should include assessments of the musculoskeletal and neurologic systems and may involve consultations with physical or occupational therapists or specialists such as neurologists, orthopedists, or rheumatologists as deemed necessary.3
Physiologic Changes and Concomitant Diseases in the Elderly
Increasing age is accompanied by physiologic changes, and these changes are important to identify, as they impact the safety and efficacy of many pain treatment modalities. Some of the age-related physiologic changes noted in elderly patients include decreased cardiac output, smaller muscle mass, increased body fat, decreased plasma proteins, and reduced hepatic and renal function.4 Thus, pharmacokinetic parameters such as drug distribution, metabolism, and elimination will be affected by medications that are heavily involved in these processes. Many opioids are involved in some of these pharmacokinetic processes, and, as a result, elderly patients are generally more sensitive to opioid analgesics compared to younger patients and typically require smaller initial doses with a slow titration as needed. Many opioids depend on liver metabolism for efficacy. Morphine and meperidine are both significantly extracted by the liver, and a reduction in hepatic blood flow due to aging, cirrhosis, and/or heart failure may necessitate a lowering of the dose. Failure to lower the dose can increase levels of opioid in the plasma and lead to adverse drug reactions (ADRs). In addition, the metabolites of morphine undergo renal elimination and can lead to further toxicities in cases of renal dysfunction. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), which cause afferent vasoconstriction in the kidneys, may precipitate renal failure in patients who receive these agents and are dehydrated. Slow titrations of other pain medications, such as propoxyphene and tramadol, are also warranted, particularly in elderly patients with reduced renal function.4
Concomitant disease states in older adults may also impact drug selection for pain management. NSAIDs generally are avoided in patients with peptic ulcer disease owing to their propensity to exacerbate the gastrointestinal (GI) condition via nonselective cyclo-oxygenase (COX) inhibition. Use of the selective COX-2 inhibitor celecoxib may minimize GI irritation; however, in light of recent data surrounding the increased risk for cardiovascular events in patients receiving chronic treatment with COX-2 inhibitors, celecoxib should be used cautiously in the elderly population, especially in those with significant cardiovascular disease.8 Acetaminophen is a commonly used pain management modality; however, cautious use is warranted in patients with liver disease and/or a history of alcohol abuse, due to its significant hepatic involvement. Opioids, corticosteroids, and NSAIDs commonly cause CNS effects such as dizziness and drowsiness, which can pose an increased risk for falls. Because corticosteroids can worsen hypertension and diabetes mellitus, and lead to osteoporosis, the lowest dose of a corticosteroid should be used. Thus, before selecting a pain management regimen, consideration for age-related physiologic changes and underlying health conditions is warranted.
Principles of Drug Selection and Consideration for DrugñDrug Interactions
The AGS acknowledges the importance of balancing risks and benefits upon medication selection for pain management in the elderly. Acetaminophen is typically considered a first-line agent for the treatment of pain, especially in older adults, as it is regarded as generally safe if used appropriately (i.e., no more than 4 g per day). After acetaminophen, anti-inflammatory drugs may be considered, followed by nonopioid pain-modulating drugs and finally opioids. However, the AGS recognizes that acetaminophen may not be appropriate for a patient experiencing pain due to inflammation and that many of these treatment modalities, especially opioids, may be ineffective to treat diabetic peripheral neuropathy, which is often best managed with anticonvulsant therapy. Thus, determination of the type of pain (i.e., somatic, visceral, neuropathic) through a thorough pain assessment is essential for selecting the appropriate treatment modality to achieve effective pain management.3
Drugñdrug interactions are important to screen for in the elderly population to avoid the potential for unnecessary ADRs and compromised efficacy of the medications. Angiotensin-converting enzyme inhibitors such as lisinopril and enalapril cause efferent vasodilation in the kidneys and can lead to worsening of renal dysfunction in older adults who are receiving concomitant high-dose NSAIDs for pain management. Patients who are receiving combination products such as propoxyphene or hydrocodone with acetaminophen should be counseled about minimizing acetaminophen intake to no more than 4 g per day to prevent liver damage, especially if it is determined the patient is taking adjunctive acetaminophen therapy for breakthrough pain. In addition, patients receiving tramadol concomitantly with a selective serotonin reuptake inhibitor such as paroxetine are at increased risk for serotonin syndrome and seizures.
Consequences of Pain Management
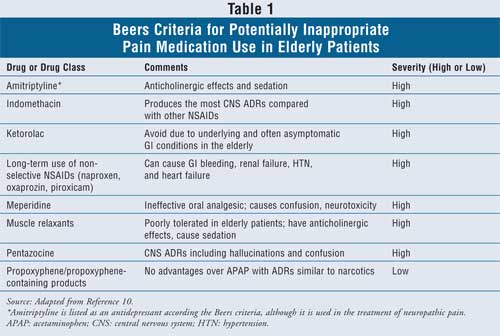
A 2001 case-control study assessed the incidence of adverse drug events (ADEs) among nursing home residents. A total of 226 residents experienced a preventable ADE, and opioid medication use, among others, was considered an independent risk factor for preventable ADEs. In addition, the number of scheduled medications was associated with a higher risk for ADEs, increasing the risk with more medications.9 Preventable ADEs include depression, falls, immobility, constipation, hip fractures, and confusion.10 To decrease the incidence of ADEs, especially those that are preventable, one approach has been the development of the Beers criteria to assess inappropriate medication use in the elderly. These criteria are generated from a consensus panel of experts who monitor the safe and effective use of medication in the elderly along with prescribing patterns and the evaluation of health outcomes. In 2002, the Beers criteria were updated and currently include 48 medications or medication classes that are generally accepted as inappropriate for use in the elderly based on clinical expertise and an extensive review of the literature. The criteria also include a rationale for identifying the medications as inappropriate as well as a ranking of their severity (i.e., high or low) with regard to use in the elderly population. Pain management options included as part of the Beers criteria are listed in Table 1. The presence of significant ADRs and/or exacerbation of underlying disease states typically accounts for these agents being classified under the Beers criteria. 10-12
Treatment of Opioid-Induced Adverse Effects
Opioid therapy may be effectively used in the elderly population with appropriate monitoring for efficacy and safety. Use of opioids, especially with chronic use, may cause ataxia, falls, dizziness, pruritus, sedation, impaired concentration, and constipation.3 Elderly patients may confuse these ADRs, especially constipation, with the normal aging process. Pharmacists are in an ideal position to appropriately counsel patients about potential ADRs and possible methods to reduce these effects.
Patients often turn to OTC methods or home remedies to treat constipation. Use of fiber and other bulk-forming laxatives such as methylcellulose and psyllium for opioid-induced constipation is not recommended. Obstruction may result from failure of the colon to stretch and allow the passage of stool due to the effects of the opioid. Chronic use of stimulant laxatives such as bisacodyl is currently part of the Beers criteria for inappropriate use in the elderly due to the risk for bowel dysfunction and dependency. These agents are also associated with the risk for fluid and electrolyte imbalances with chronic use. However, short-term use of a stimulant laxative may be appropriate for some patients. Saline laxatives such as magnesium citrate should be used very cautiously in elderly patients, especially in those with underlying disease states such as renal dysfunction, hypertension, and heart failure. Magnesium citrate can lead to hypermagnesemia in the setting of compromised renal function, and it contains high concentrations of sodium, which can be deleterious to the heart. Mineral oil is not recommended for use in the elderly, especially those who are bedridden, as it is associated with the risk for lipoid pneumonia if the product is aspirated. Glycerin suppositories are a possible treatment option and work by producing a local irritant effect to cause a bowel movement. This may be ideal for patients with comorbidities who are receiving multiple medications to avoid the risk for disease exacerbation and/or drugñdrug interactions. Stool softeners such as docusate sodium, hence their name, work to soften the stool to make passage easier. These agents are often given in combination with a stimulant laxative to soften the stool before evacuation. They are generally recommended for patients who should not strain, such as those with severe hypertension or cardiovascular disease or who have had surgery.13,14
Role of the Pharmacist
Since pharmacists are the most accessible health care professionals, they are at the forefront of providing appropriate care to older adults who are experiencing pain. However, pharmacists may be reluctant to fill prescriptions for opioids for fear of patient misuse and abuse as well as the risk for legal ramifications. These barriers to receiving medications can lead to continuous suboptimal treatment of pain in the elderly. Thus, knowledge of guidelines and pain management algorithms is important to ensure that patients are adequately and appropriately treated for pain. In addition, pharmacists are encouraged to become familiar with common techniques used for forged prescriptions as well as with medications in various areas of the country that are often abused. 7
Recognizing that pain is a commonly undertreated condition in the elderly and that barriers to treatment often exist, pharmacists may educate older adults about the appropriate use of medications to provide adequate relief in order to improve QOL and maintain full functional capacity. Additionally, patient reports of pain should be taken seriously, and referral to the primary care provider should be encouraged. Recommendations for OTC pain medications can provide the opportunity for pharmacists to ask more questions, as older patients often have misconceptions about pain management and may be inappropriately treated for their condition. Screening for drugñdrug and drugñdisease interactions is important to avoid a preventable ADE. Pharmacists may be queried about self-treatment options for ADRs associated with pain regimens. Thus, knowledge of common ADRs along with when to appropriately self-treat and when to refer to a health care provider is important. Pain is a real phenomenon in older adults. However, understanding barriers to care and age-related physiologic changes as well as recognizing concomitant disease states and medications can improve pain management outcomes in the elderly population.
R eferences
1. Cooner E, Amorosi S. The Study of Pain in Older Americans . New York, NY: Louis Harris and Associates; 1997. Study No. 628200.
2. Ferrell BA. Pain evaluation and management in the nursing home. Ann Intern Med. 1995;123:681-687.
3. AGS Panel on Persistent Pain in Older Persons. The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50:S205-S224.
4. Prowse M. Postoperative pain in older people: a review of the literature. J Clin Nurs. 2006;16:84-97.
5. Gloth FM. Pain management in older adults: prevention and treatment. J Am Geriatr Soc. 2001;49:188-199.
6. Chakour MC, Gibson SJ, Bradbeer M, et al. The effect of age on A-delta and C-fibre thermal pain perception. Pain. 1996;64:143-152.
7. Finley RS. Treating chronic nonmalignant pain: issues and misconceptions. U.S. Pharmacist. 2002. Available online at: www.uspharmacist.com/print.asp?page=ce/nonmalignant/default.htm. Accessed February 16, 2007.
8. Solomon SD, McMurray JJ, Pfeffer MA, et al. Cardiovascular risk associated with celecoxib in a clinical trial for colorectal adenoma prevention. N Engl J Med. 2005;352:1071-1080.
9. Field TS, Gurwitz JH, Avron J, et al. Risk factors for adverse drug events among nursing home residents. Arch Intern Med. 2001;161:1629-1634.
10. Fick DM, Cooper JW, Wade WE, et al. The Beers criteria for potentially inappropriate medication use in older adults. Arch Intern Med. 2003;163:2716-2724.
11. Aparasu RR, Mort JR. Inappropriate pre639-642.scribing for the elderly: Beers criteria-based review. Ann Pharmacother. 2000;34:338-346.
12. Jano E, Aparasu RR. Healthcare outcomes associated with Beers' criteria: a systematic review. Ann Pharmacother. 2007;41:438-448.
13. Yuan CS, Foss JF. Antagonism of gastrointestinal opioid effects. Reg Anesth Pain Med. 2000;25:639-642.
14. Curry CE Jr., Butler DM. Constipation. In: Berardi RR, Kroon LA, McDermott JH, et al, eds. Handbook of Nonprescription Drugs: An Interactive Approach . 15th ed. Washington, DC: American Pharmacists Association; 2006:299-326.
To comment on this article, contact editor@uspharmacist.com.
†





