US Pharm.
2007;32(10):61-63.
Type 2 diabetes mellitus is a chronic and
progressive syndrome characterized by several metabolic factors that
eventually lead to hyperglycemia. The development and progression to type 2
diabetes significantly increases morbidity and mortality, most often due to
chronic complications.1 In the United States, type 2 diabetes has
reached epidemic proportions. In 2005, approximately 21 million adult
Americans had diabetes, and it was estimated that an additional 1.5 million
new cases would be diagnosed that same year.2 The prevalence of
diabetes is only expected to rise. The financial impact of this disease state
is staggering, with an estimated $132 billion directed toward the total cost
of care in 2002.3 This article highlights major risk factors that
are commonly associated with type 2 diabetes.
The development of diabetes tends to be
insidious. The presence of risk factors may precede the actual onset of the
disease by several years. Many times, patients may have diabetes for several
years before symptoms are apparent or a diagnosis is made. In some cases,
patients have identifiable risk factors for the disease that are not addressed
in a medical setting, or risk factors are addressed but not aggressively
enough. Decreasing the risk of progression to diabetes may greatly lower the
development of complications such as cardiovascular disease, retinopathy,
nephropathy, and neuropathy. Pharmacists have the ability and obligation to
educate patients and be further involved in their care when appropriate.
Identifying risk factors to aid primary prevention is an important
intervention needed to decrease the associated morbidity and mortality.
Prediabetes
Prediabetes
refers to blood glucose impairment that is not yet classified as type 2
diabetes. Without intervention, the risk of progression to overt diabetes is
high. The American Diabetes Association (ADA) defines prediabetes as either an
impaired fasting plasma glucose of 100 to 125 mg/dL or an impaired glucose
tolerance as determined by a two-hour post–glucose load plasma glucose of 140
to 199 mg/dL after taking 75 g of anhydrous glucose dissolved in water.1
Pathogenesis
The underlying pathway for
development of type 2 diabetes is unclear; however, experts postulate
abdominal obesity and insulin resistance is a main contributor.4
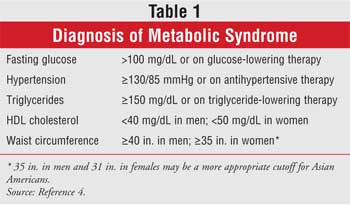
Metabolic syndrome is commonly associated with insulin resistance and
abdominal obesity and is a common risk factor for diabetes and cardiovascular
disease. There are several definitions for diagnosis of the metabolic
syndrome. The Adult Treatment Panel III (ATP III)definition is commonly used
in clinical practice due to clinical simplicity.4 It has been
modified slightly and supported by the American Heart Association and the
National Heart, Lung, and Blood Institute. According to these criteria,
metabolic syndrome is diagnosed in individuals who meet at least three of the
criteria identified in Table 1.4
The underlying pathogenic changes that take
place predispose a patient to several metabolic alterations, including
abnormal changes to glycemia, decreased HDL cholesterol levels, increased
small dense atherogenic LDL cholesterol levels, increased triglyceride levels,
hypertension, and hypercoagulable states.4 Genetic
predisposition may have a role; however, lifestyle choices appear to have a
tremendous role in development. Metabolic syndrome is often apparent in
patients with increased weight, sedentary lifestyle, and a positive smoking
history.5
Risk Factors
While there are several
modifiable risk factors associated with diabetes, it is important to identify
those that are nonmodifiable. The development of diabetes is often linked
within families. People who have a first- or second-degree relative with
diabetes have an increased genetic predisposition for the disease. Increased
age is also associated with diabetes development. The highest incidence of
diabetes occurs in those ages 65 to 74.6 Although type 2 diabetes
was once traditionally associated with advanced age, due to changes in
American culture (including increased sedentary lifestyles and high-calorie,
high-fat diets), the incidence has risen in adolescents and younger adults.
Persons of certain ethnic origins have a disproportionately increased risk of
developing type 2 diabetes. Those considered at highest risk include Americans
of African, Asian, Latino/Hispanic, and Native American or Pacific Islander
descent1.
While some of the risk factors for diabetes
cannot be changed, there are several risk factors that can. One of the major
modifiable risk factors for the development of diabetes is obesity.4
Guidelines from the ADA recommend persons age 45 years or older be screened
for prediabetes or diabetes, especially if they are overweight.1
Younger individuals may be screened if they are overweight and have additional
risk factors.1
Obesity is often associated with a sedentary
lifestyle. The morbidity and mortality associated with obesity is concerning
considering the increase in risk of several disease states, including
hypertension, coronary heart disease, and diabetes.4,5 Overweight
(BMI = 25-30 kg/m2) and obese individuals (BMI >30 kg/m2
) have an increased risk of several disease-state risk factors. Increased
weight, especially abdominal obesity, is also associated with the metabolic
syndrome through several proposed mechanisms associated with increased adipose
tissue mass.4
Interventions
Data support that even a moderate
decrease in weight of 5% to 10% helps to improve underlying insulin resistance.
4,7-9 Risk of progression to type 2 diabetes has been observed to
decrease with decreasing weight; increasing physical activity; eating a diet
that is low in saturated and trans fat, low in cholesterol, and high in fiber;
minimizing alcohol consumption; and quitting smoking. Patients at risk for
diabetes should be encouraged to engage in at least 30 minutes of moderately
intense physical activity most days of the week.1,4
There are several studies that support
lifestyle intervention as an effective method in decreasing the risk of
diabetes. The Diabetes Prevention Program (DPP) Trial randomized 3,234
patients with prediabetes to receive pharmacologic or nonpharmacologic
intervention to determine if the progression to overt diabetes could be halted
in those with impaired glucose tolerance. Of the three groups included in the
study, one received metformin 850 mg twice daily with a standard regimen of
diet and exercise. Another made intensive lifestyle changes aimed at
decreasing weight by 7% utilizing a low-calorie, low-fat diet and maintaining
moderate physical activity at 150 minutes per week. The third group received
placebo tablets twice daily as well as a standard regimen of diet and exercise.
7 After an average follow-up time of 2.8 years, there was a 58% and 31%
reduction in the progression to diabetes, compared to placebo in the intensive
lifestyle modification group and metformin groups, respectively.7
The results of this study support the rationale that intensive lifestyle
changes are effective in decreasing the progression to diabetes in high-risk
patients.
Additional data from other trials, such as
the Finnish Diabetes Prevention Program, support that a relatively small
decrease in weight (in this case 5%) through lifestyle intervention still has
a significant impact in decreasing the risk of progression to diabetes.8
For patients in whom diet and exercise are not enough to decrease weight,
other weight loss options may be available. The XENical in the Prevention of
Diabetes in Obese Subjects (XENDOS) study randomized 3,305 obese individuals
to receive placebo or orlisat in addition to a low-calorie, limited-fat diet
and encouragement to participate in regular physical activity. At enrollment,
approximately 40% of individuals had impaired glucose tolerance. At the end of
the four-year study period, there was a 37.2% decrease in the incidence of
diabetes in patients with preexisting glucose intolerance who received active
drug and lifestyle modifications versus placebo and lifestyle modifications.
9 For some patients with severe obesity or who have obesity-related
complications, bariatric surgery may also be an option.10
Persons with a past history of impaired
fasting glucose or impaired glucose tolerance are also at high risk of
progression to diabetes later in life. Although it may take several years, the
predictive risk is high unless interventions are made. Included in this risk
category are women with a history of gestational diabetes, which occurs in up
to 14% of pregnancies.11 Even if normoglycemia returns postpartum,
these woman have an increased lifetime risk of future development of diabetes.
11 Women at highest risk are those who have a family history of
diabetes; are overweight or obese at the beginning of pregnancy; have
previously had impaired glucose tolerance; have had a baby weighing more than
9 lb.; or had previous glycosuria.1 Women meeting these criteria
should be screened at their first prenatal visit.1 Women with a
history of polycsytic ovary syndrome (PCOS) also have an increased risk of
impaired glucose tolerance and diabetes.12 Among other factors,
PCOS is often associated with overweight, obesity, and insulin resistance; and
although difficult, a decrease in weight will improve glycemic control.
Metformin and thiazolidenediones are also used in this patient population to
improve blood sugar and insulin sensitivity.12 Women with a lower
risk or those who test negative should be evaluated again in the 24th to 28th
week of pregnancy.1
Once an individual is considered at high
risk for the future development of diabetes, aggressive interventions are
needed to decrease the risk of progression. In addition to lifestyle
intervention, which have a primary role, there are also pharmacological
options available. As mentioned previously, metformin, as used in the DPP
study, is proven to be efficacious in individuals with prediabetes. The
STOP-NIDDM study demonstrated acarbose to be effective in individuals with
impaired glucose tolerance.13 This is a reasonable option in
patients who have postprandial elevations in glucose. Patients prescribed
these agents should be monitored to ensure safety and efficacy.
Metformin may be started at 500 or 850 mg
once daily and titrated to a maximum effective dosage of 2,550 mg daily in
divided doses.14 Gastrointestinal side effects are the most common
dose-limiting factor and may be improved with the extended-release formulation.
14 While the development of lactic acidosis is rare, it can be
life-threatening. Because of this increased risk, metformin should be used
with caution in patients with severe hepatic disease, alcoholism, previous
history of lactic acidosis, or conditions predisposing them to lactic acidosis.
14,15 An increased risk of lactic acidosis is particularly concerning in
patients with a history of renal disease who are receiving metformin. These
patients should be monitored carefully while on metformin therapy. Metformin
is contraindicated in males and females with serum creatinine levels of
greater than 1.5 mg/dL and greater than 1.4 mg/dL, respectively.15
Renal function should be monitored prior to initiation and at least annually
thereafter.15
Acarbose is often started at 25 mg right
before meals and may be slowly titrated to 100 mg three times daily.14
Dose-limiting side effects are often gastrointestinal and are a main reason
for discontinuation of the agent. Higher doses may increase serum
transaminases; these should be checked every three months for the first year,
then periodically. The dose should be decreased or discontinued if there is an
increase in transaminases. Caution should be used in patients with renal
disease. Acarbose should not be used in patients with severe liver
disease, those with inflammatory bowel disease, or patients with other chronic
intestinal conditions.16
The Role of the Pharmacist
Pharmacists are encouraged to
inform patients that although drug therapy is a viable option in prediabetic
patients, it should always be used as an adjunct to lifestyle intervention.
Pharmacists' awareness that improvement in diabetes-associated risk factors is
a multifactorial approach is vital. Most of the afore-mentioned interventions
help to decrease the risk of other conditions such as cardiovascular disease
and hypertension. Patient education is an important intervention. For some
patients, an understanding of the disease state and risk of complications is
enough incentive to be better invested in their own care. Patients should have
a clear understanding of the risk factors that predispose them to diabetes and
ithe ntervention strategies available for prevention and treatment. In order
to implement and sustain lifestyle interventions, patients may need
specialized care within a multidisciplinary team approach.
References
1. Clinical Practice
Recommendations 2007. American Diabetes Association. Diabetes Care.
2007;30(suppl 1):S4-S65.
2. American Diabetes Association.
Total prevalence of diabetes & pre-diabetes. Available at:
diabetes.org/diabetes-statistics/prevalence.jsp. Accessed August 16, 2007.
3. Centers for Disease Control and
Prevention. National diabetes fact sheet: general information and national
estimates on diabetes in the United States, 2003. Rev ed. Atlanta, GA: U.S.
Department of Health and Human Services, Centers for Disease Control and
Prevention, 2004. Available at: www.cdc.gov/diabetes/pubs/pdf/ndfs_2003.pdf.
Accessed August 16, 2007.
4. Grundy SM, Cleeman JI, Daniels SR,
et al. Diagnosis and management of the metabolic syndrome: an American Heart
Association/National Heart, Lung, and Blood Institute scientific statement.
Circulation. 2005;112;2735-2752.
5. Hu FB, Manson JE, Stampfer MJ, et
al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N
Engl J Med. 2001;345:790-797.
6. Centers for Disease Control and
Prevention. Incidence of diagnosed diabetes per 1000 population aged 18-79
years, by age, United States, 1980-2005. Available at:
www.cdc.gov/diabetes/statistics/incidence/fig3.htm. Accessed August 16, 2007.
7. Diabetes Prevention Program
Research Group. Reduction in the incidence of type 2 diabetes with lifestyle
intervention or metformin. N Engl J Med. 2002; 346:393-403.
8. Tuomilehto J, Lindström J,
Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in
lifestyle among subjects with impaired glucose tolerance. N Engl J Med.
2001;344:1343-1350.
9. Torgerson JS, Hauptman J, Boldrin
MN, Sjöström L. XENical in the prevention of diabetes in obese subjects
(XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle
changes for the prevention of type 2 diabetes in obese patients. Diabetes
Care. 2004;27:155-161.
10. Folli F, Pontiroli AE,
Schwesinger WH. Metabolic aspects of bariatric surgery. Med Clin N Am.
2007;91:393-414.
11. Jovanovic L, Pettitt DJ.
Gestational diabetes mellitus. JAMA. 2001; 286:2516-2518.
12. Ehrmann DA. Polycystic ovary
syndrome. N Engl J Med. 2005;352:1223-1236.
13. Chiasson J, Josse RG, Gomis R, et
al. Acarbose treatment and the risk of cardiovascular disease and hypertension
in patients with impaired glucose tolerance: facts and interpretations
concerning the critical analysis of the STOP-NIDDM Trial data. JAMA.
2003;290:486-494.
14. Nolte MS, Karam JH. Pancreatic
hormones and antidiabetic drugs. In: Katzung BG, ed. Basic and Clinical
Pharmacology. 10th ed. New York, NY: Mc-Graw Hill; 2007:697-698.
15. Glucophage/Glucophage XR [package
insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2006.
16. Precose [package insert]. West
Haven, CT: Bayer Pharmaceutical Corporation; 2004.
To comment on this article, contact
editor@uspharmacist.com.





