US Pharm. 2008;33(2):22-25.
Warfarin, the oral
anticoagulant most frequently used to control and prevent thromboembolic
disorders, is increasingly common among seniors.1,2 The debate
continues, however, regarding the risks associated with therapy, even though
its use has been extensively studied in the geriatric population.3
In fact, the black box warnings for warfarin therapy include age over 65
years as a specific risk factor for bleeding. While seniors derive
the greatest benefit from anticoagulant therapy, the elderly demonstrate an
enhanced responsiveness to warfarin, and pharmacists need to provide
monitoring that is delivered with greater vigilance in this population.
1,4
In the U.S., approximately two
million individuals use warfarin as maintenance therapy in the treatment of
atrial fibrillation or to prevent blood clotting after a heart attack, stroke,
fracture, or surgery.5 Warfarin sodium (Coumadin), introduced into
the American marketplace in 1954, continues to rank highly among prescription
medications dispensed--over 30 million in 2006.6-8 From patient to
patient, dosages vary widely, with a tenfold difference in strength between
the least potent and most potent tablet. Even for an individual patient, the
dosage is often adjusted to accommodate a response due to interactions with
other medications, nutritional supplements, herbal products, food, and
alcohol, resulting in time-intensive management for both health care provider
and patient alike. Arriving at the specific dose that avoids hemorrhagic
complications while at the same time achieving sufficient suppression of
thrombosis requires a thorough understanding of the drug's unique
pharmacology.
Anticoagulation clinics have
been operating for over three decades to manage patients receiving warfarin
with its complex doseñresponse relationship; however, safe and effective use
remains a challenge due to the multifaceted potential for altered response to
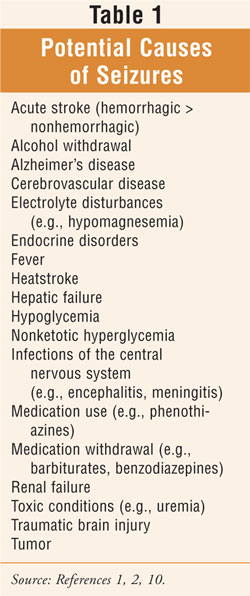
therapy (TABLE 1).2,6,9 This difficulty underscores the need
for all pharmacists involved in the care of the warfarin patient to closely
monitor therapy--from the anticoagulation pharmacist, to the dispensing
pharmacist, to the consultant pharmacist, to the hospital pharmacist--across
all health care settings so that the continuum of care does not falter. This
notion of comprehensive monitoring and the significance of the pharmacist's
involvement in the outcome of the warfarin patient is represented in the
following tenet of pharmacotherapy: "Careful observation of a patient's
response to treatment is necessary to confirm efficacy, prevent, detect, or
manage adverse effects, assess compliance, and determine the need for dosage
adjustment or discontinuation of drug therapy."10
Emergency Department Visits
A recent large
study looking at emergency department (ED) visits for the adverse events among
persons 65 years or older found that, aside from the small percentage (3.6%)
of visits for adverse drug events (ADEs) associated with medications
considered to be always potentially inappropriate in the elderly (i.e.,
according to the Beers criteria), approximately one-third of all visits were
for adverse events associated with warfarin (17.3%), insulin (13.0%), and
digoxin (3.2%).11,12 The researchers reported that, considering
frequency of prescribing, the risk of ED visits from warfarin, insulin, and
digoxin is 35 times greater than the risk of visits from Beers criteria
medications.12 The researchers suggested that performance measures
and interventions targeting warfarin, insulin, and digoxin use could prevent
more ED visits for adverse events.12†
Key Issues and Adverse Events
Seniors may be more
prone to excessive anticoagulation secondary to comorbidities, nutritional
deficiencies, and multiple drug interactions.1 Bleeding is the most
common complication of warfarin therapy, contributing to medication-related ED
visits, morbidity, mortality, and increased health care expenditures. The
increased risk of falls in this population is also a factor related to
bleeding.1 Pharmacists should note that warfarin is contraindicated
in a patient who has a history of falls or is a significant fall risk.13
Bleeding: The
primary adverse effect from warfarin is bleeding.1 The most
powerful risk factor for bleeding is intensity of anticoagulation (e.g.,
international normalized ratio [INR] > 4.0); others include age greater than
65; initiation of therapy (first few weeks), comorbidities (cerebrovascular
disease, renal failure, malignancy); a history of gastrointestinal bleeding;
concurrent antiplatelet drug or NSAID use; recent surgery, trauma, or fall;
heavy alcohol use; and unstable anticoagulation response.1 Patients
with two or three risk factors have a considerably higher incidence of
warfarin-associated bleeding compared with those with one or none.14
Changes in dosage should be made more cautiously in the geriatric patient.
1 Reference 13 provides thorough charts for INR ranges (based on
indication) and the management of elevated INR (with no significant bleeding,
serious bleeding, or life-threatening bleeding), an extensive list of warfarin
drug interactions (including CYP-450 information), and specific geriatric
dosing and administration issues.13
The reader is reminded of the
importance of postmarketing surveillance with newer drugs; its significance
was illustrated by the drug celecoxib, which showed no interactions in phase 2
studies but was subsequently suspected of potentiating the effect
of warfarin in several case reports.15 Furthermore, the clinician
should not overlook the potential interactions with less well-regulated
herbal medicines. Due to these considerations, the INR should be measured
more frequently when virtually any drug or herbal medicine is added
to or withdrawn from the medication regimen of a warfarin patient.14
Additionally, it is considered a generally good practice to monitor response
with additional INR determinations in the period immediately following
discharge from the hospital.16
Combination Aspirin and
Warfarin Therapy: Following an acute coronary syndrome (i.e., clot
formation subsequent to plaque rupture), anticoagulation with warfarin is
considered in addition to aspirin in selected patients (e.g., left ventricular
thrombus; extensive ventricular wall motion abnormalities on cardiac
echocardiogram; history of thromboembolic disease or chronic atrial
fibrillation).17 Patients receiving combination warfarin and
aspirin therapy are at increased risk for minor and major bleeding.18†
With regard to adherence, individuals on this combination therapy have been
shown to be two to three times more likely to discontinue their treatment.
18 Even though warfarin in combination with aspirin is superior to
aspirin monotherapy, it is not currently recommended as a preferred regimen in
practice guidelines by any professional association in patients other than
those mentioned earlier.18
Nonhemorrhagic Adverse
Effects: The most important side effect of warfarin, other than
hemorrhage, is skin necrosis. While uncommon, its appearance is sudden in
onset, is causedby extensive thrombosis of venules and capillaries within
subcutaneousfat, and is recognized by patchy skin necrosis observed
on the third to eighth day of therapy initiation.14 While the
complete pathogenesis of this complication is uncertain and reports link
warfarin-induced skin necrosis and protein C deficiency and, less
commonly, protein S deficiency, this condition also occurs in
patients without these issues.14 Since warfarin is considered
contraindicated in these individuals and long-term treatment with
heparin is inconvenient and associated with osteoporosis, warfarin should be
discontinued immediately, vitamin K should be administered, and full-dose
unfractionated heparin or low-molecular-weight heparin therapy should be
initiated.1 †Warfarin should be restarted with extreme caution, if
at all, in patients with a history of skin necrosis.1
Medication Errors:
A medication error is certainly one of many circumstances that can potentially
alter a desired therapeutic outcome of drug therapy (TABLE 1). In
general, prescribing errors are common, and the elderly are especially at risk.
9 A drug error most commonly results from a patient's confusion about
how to take medication.9 Dosing instructions should therefore be
completely explained. Convenient, safe packaging with clear labeling should be
provided, proper storage requirements discussed, and expiration date noted.
Nonchildproof packaging should be supplied to a senior to avoid difficulty in
opening, as long as children are not likely to have access to the product.
9 Furthermore, pharmacists are encouraged to maintain a complete problem
list and obtain information regarding all medications that are being
prescribed by all involved health care providers; OTCs, nutritional
supplements, and herbal therapies should also be included.
Nutritional Factors:
Changes in the usual intake of vitamin K may cause variable anticoagulation
effects of warfarin.19 The dietary requirement for vitamin K is
about 100 mcg daily, and while deficiency of vitamin K from inadequate diet is
extremely rare, a patient with a borderline intake may become deficient in an
acute situation where food is withheld or appetite is diminished and
antibiotic therapy is required.20 Exquisite sensitivity to
warfarin, not uncommon in the elderly, disappears when the dietary intake is
supplemented with 80 to 150 mcg of vitamin K daily.20 With
appropriate and steady supplementation, the dietary intake of vitamin K
becomes a minor consideration in the overall equation, with sensitivity to
warfarin returning to normal.20
Reference 1 provides a
thorough listing of potential warfarin interactions with herbal and
nutritional products and a table noting the vitamin K content of selected
foods.1
Pharmacogenetics:
Pharmacogenetics refers to variations in medication response secondary to
genetic makeup. It has been predicted that future personalization of warfarin
dosing using technology to determine genetic information can save over one
billion health care dollars annually in the U.S.21,22 Along these
lines, in August of 2007, the FDA announced a new label for warfarin that for
the first time discussed the genetic factors related to therapy. Under the
"Precautions" heading in the package insert, it states, "Numerous factors,
alone or in combination including changes in diet, medications, botanicals,
and genetic variations in the CYP2C9 and VKORC1 enzymes may influence
the response of the patient to warfarin."23 About 10 percent
of the difference in patients' responses to warfarin is attributed to
variations in a gene encoding the CYP2C9 enzyme that metabolizes warfarin.
22,24 The recently identified gene, vitamin K epoxide reductase,
or VKORC1, is a key component in the clotting process and the primary target
of warfarin.22,25
Conclusion
Comprehensive monitoring, one of the
principles of pharmacotherapy, is especially important as part of the
pharmaceutical care plan for the warfarin patient. By understanding potential
warfarin adverse events, including pharmacogenetic issues and sources and
manifestations of medication errors, the pharmacist may be better equipped to
identify, resolve, and prevent them. Awareness of key issues related to
warfarin therapy can provide for a more tailored medication regimen. There
continues to be confirmation regarding the notion that, among seniors,
strategies to decrease ADEs in general should include a focus on warfarin.
REFERENCES
1. Haines ST, Zeolla M, Witt DM. Venous thromboembolism. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 6th ed. New York: McGraw-Hill; 2005:389-395.
2. Horton JD, Bushwick BM. Warfarin therapy: evolving strategies in anticoagulation. Am Fam Physician. 1999. Available at: www.aafp.org/afp/990201ap/635.html. Accessed January 11, 2008.
3. Levine MN, Raskob G, Beyth RJ, et al. Hemorrhagic complications of anticoagulant treatment: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:287S-310S.
4. Lindblad CI, Gray SL, Guay DR, et al. Geriatrics. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 6th ed. New York: McGraw-Hill; 2005:107.
5. Rieder MJ, Reiner AP, Gage BF, et al. Effect of VKORC1 haplotypes on transcriptional regulation and warfarin dose. N Engl J Med. 2005;352:2285-2293.
6. Lodwick AD, Sajbel TA. Improving warfarin therapy for an elderly, poor population. Drug Benefit Trends. 2000. Available at: www.medscape.com/viewarticle/409902. Accessed January 11, 2008.
7. The Top 200 Prescription Drugs of 2005. Pharmacy Times. May 2006. Available at: www.pharmacytimes.com/issues/articles/2006-05_3468.asp. Accessed January 11, 2008.
8. Mathews AW. In: Milestone, FDA pushes genetic tests tied to drug. Wall Street Journal. August 16, 2007:1,A8.
9. Beers MH, Porter RS, Jones TV, et al. The Merck Manual of Diagnosis and Therapy. 18th ed. Whitehouse Station, NJ: Merck Research Laboratories; 2006:2519,2537,2543.
10. DiPiro JT, Talbert RL, Yee GC, et al., eds. Guiding Principles of Pharmacotherapy. Pharmacotherapy: A Pathophysiologic Approach, 6th ed. New York: McGraw-Hill; 2005:xxxiii.
11. Fick DM, Cooper JW, Wade WE, et al. Updating the Beers Criteria for potentially inappropriate medication use in older adults: results of a U.S. consensus panel of experts. Arch Intern Med. 2003;163:2716-2724.
12. Budnitz DS, Shehab N, Kegler SR, et al. Medication use leading to emergency department visits for adverse drug events in older adults. Ann Intern Med. 2007;147:755-765.
13. Semla TP, Beizer JL, Higbee MD. Geriatric Dosage Handbook. 12th ed. Hudson, Ohio: Lexi-Comp, Inc.; 2007:1646-1652.
14. Hirsh J, Fuster V, Ansell J, et al. American Heart Association/American College of Cardiology Foundation Guide to Warfarin Therapy. AHA/ACC Scientific Statement. Circulation. 2003. Available at: www.circ.ahajournals.org/cgi/content/full/107/12/1692. Accessed January 11, 2008.
15. Wittkowsky AK. Drug interactions updates: drugs, herbs and oral anticoagulation. J Thromb Thrombolysis. 2001;12:67-71.
16. Coumadin [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2007.
17. Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). Circulation. 2004;110:588-636.
18. Spinler SA, de Deus S. Acute coronary syndromes. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 6th ed. New York: McGraw-Hill; 2005:291-319.
19. Chessman KH, Kumpf VJ. Assessment of nutrition status and nutrition requirements. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 6th ed. New York: McGraw-Hill Inc.; 2005:2572.
20. Matulis M, Knovich MA, Owen J. Thrombotic and hemorrhagic disorders. In: Hazzard WR, Blass JP, Halter JB, et al, eds. Principles of Geriatric Medicine and† Gerontology. 5th ed. New York: McGraw-Hill, Inc.; 2003:803-817.
21. Johnson LA. DNA tests to determine warfarin dose. The Associated Press; January 13, 2007. Available at: www.washingtonpost.
com/wp-dyn/content/article/2007/01/13/AR2007011300264.html. Accessed
January 11, 2008.
22. Zagaria ME. Future technology for warfarin dosing: advances in pharmacogenetics. US Pharm. 2007;32(3):34-38. Available at: www.uspharmacist.com/index.asp?show=article&page=8_1977.htm.
23. Coumadin [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; August 2007.
24. Genetic variation alters response to common anti-clotting drug. National Institute of General Medical Sciences, National Institutes of Health, Department of Health and Human Services. Available at: www.nigms.nih.gov/News/Results/060205.htm. Accessed January 29, 2006.
25. Determining drug dose with DNA:
graduate School alumnus leads study of genetic influence on response to common
blood thinner. Available at: www.mcw.edu/display/router.asp?docid=15475.
Accessed January 29, 2007.
To comment on this article,
contact editor@uspharmacist.com.





